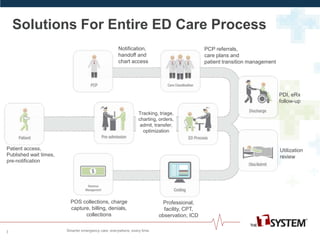
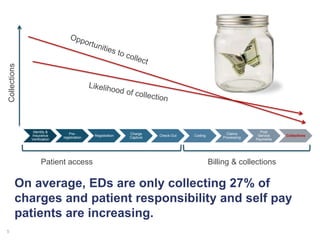
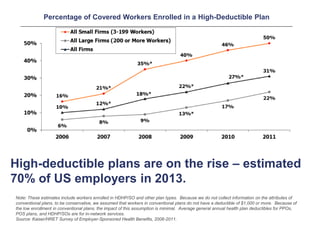
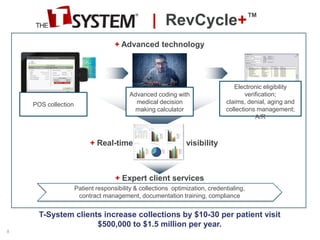
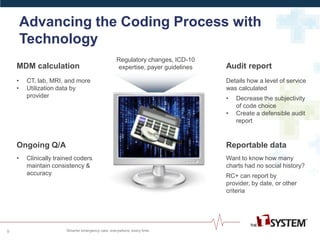
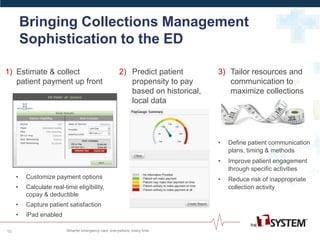
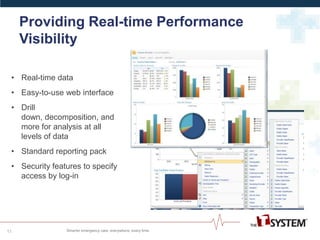
RevCycle+TM by T-System offers comprehensive revenue cycle solutions for emergency departments, improving efficiency through automation and advanced technology. The platform enhances coding accuracy, performance visibility, and patient collections, potentially increasing collections by up to $1.5 million annually for clients. With over 30 years of experience, T-System provides ongoing provider training and support in regulatory compliance and contract negotiation.