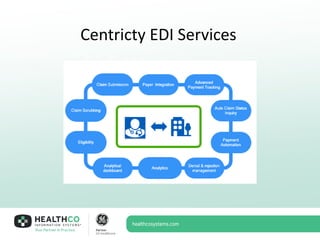
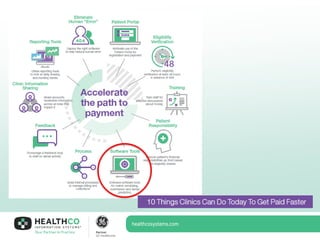
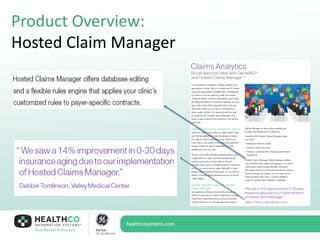
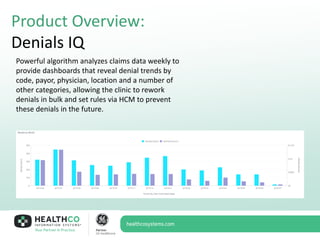
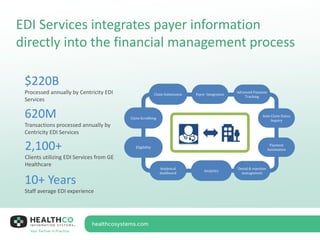
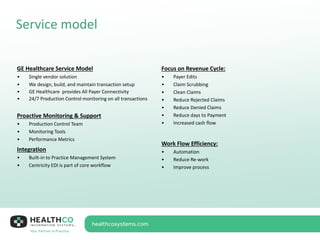
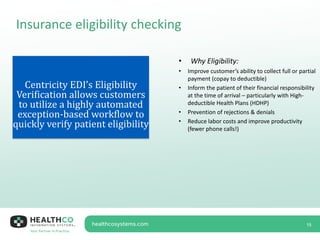
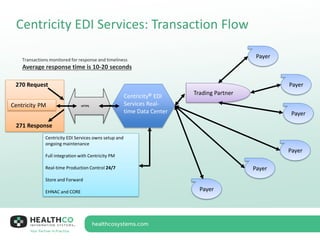
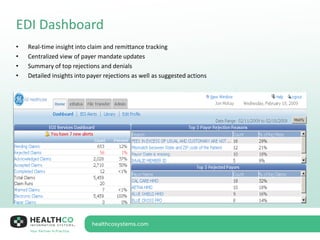
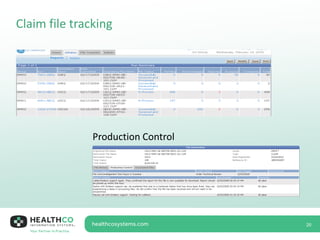
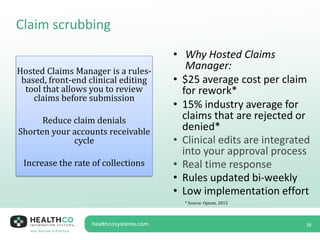
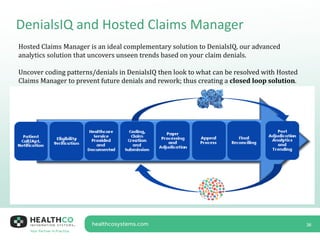
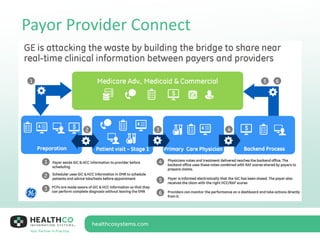
The document provides an overview of Centricity EDI Services, emphasizing its benefits for improving patient care and financial performance for independent physician practices. Key features include hosted claims management, denial analytics, and integrated eligibility verification, which together enhance workflow efficiency and reduce claim denials. The presentation outlines successful case studies demonstrating significant improvements in collections and operational efficiency after transitioning to the Centricity platform.