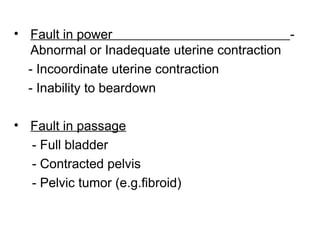
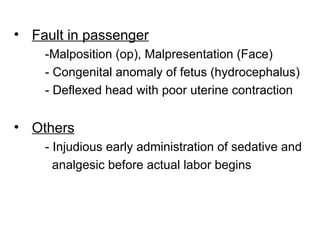
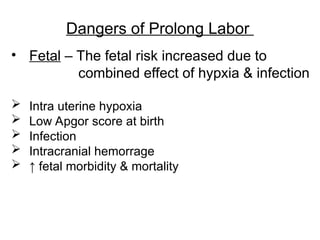
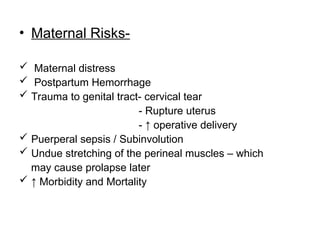
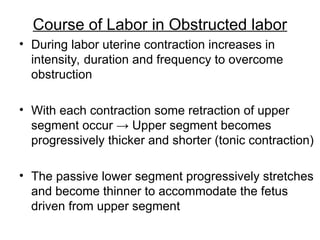
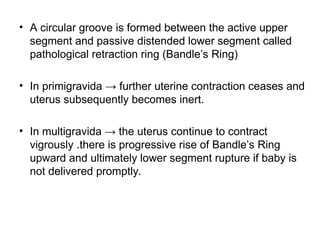
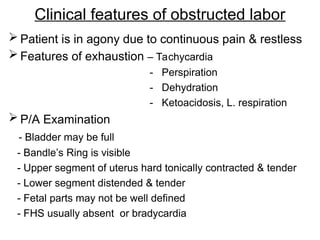
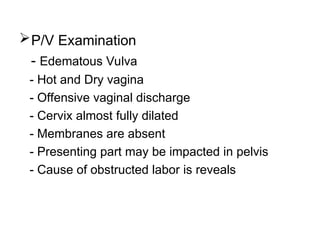
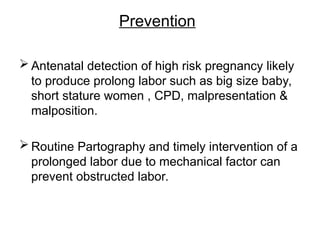
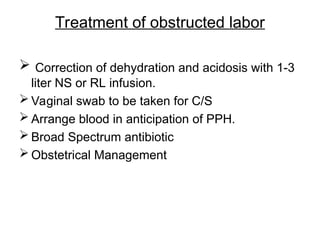
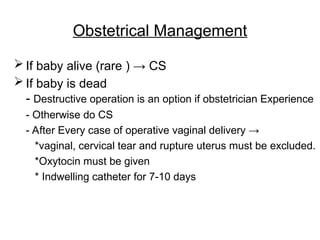
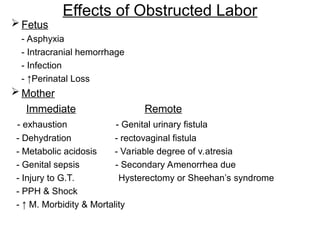
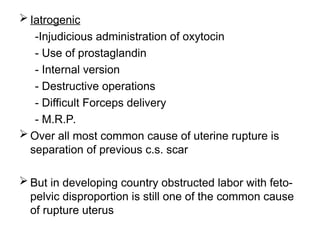
Prolonged and obstructed labor refer to complications in childbirth characterized by extended duration and mechanical obstruction despite adequate uterine contractions, respectively. Prolonged labor can lead to maternal and fetal risks such as hypoxia, infection, and increased morbidity, influenced by factors like uterine contractions, pelvic structure, and fetal positioning. Management focuses on early intervention, supportive care, and surgical options when necessary, including cesarean sections for fetal distress or obstructed labor conditions.