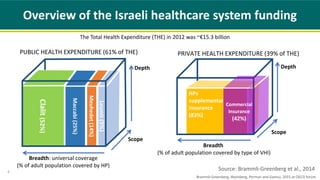
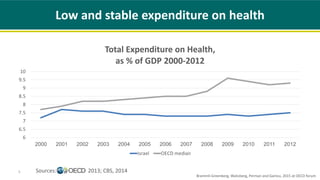
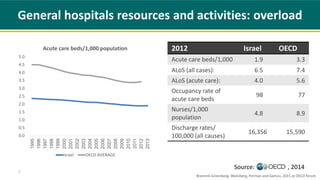
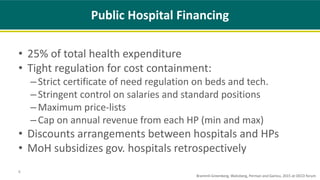
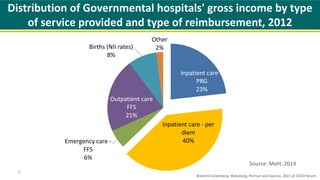
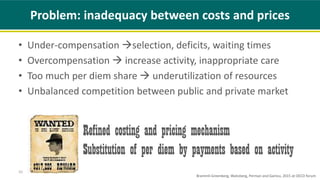
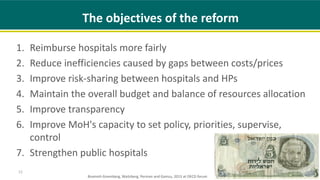
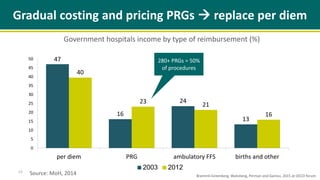
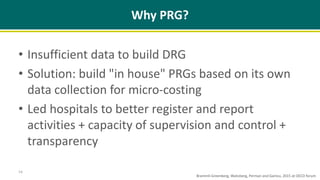
The document discusses Israel's reform of hospital reimbursement systems from a per diem model to a procedure-related group (PRG) framework to enhance fairness and efficiency. It examines the structure of the Israeli healthcare system, hospital challenges, and the objectives and advantages of the incremental PRG reform. The authors present lessons learned from the reform process and its implications for other countries considering similar healthcare financing changes.