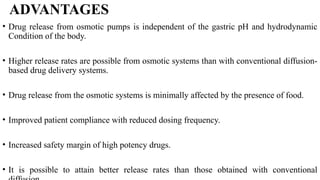
The document discusses various types of drug delivery systems, focusing on rate-controlled drug delivery mechanisms. It contrasts sustained release and controlled release systems, outlines their advantages and disadvantages, and details classifications such as rate-preprogrammed, activation-modulated, feedback-regulated, and site-specific systems. The seminar highlights advancements in drug delivery technology, emphasizing controlled drug release rates and targeting specific tissues for therapeutic benefits.