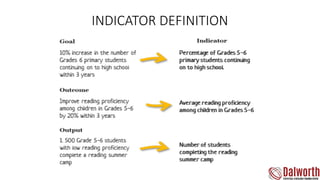
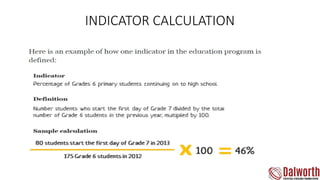
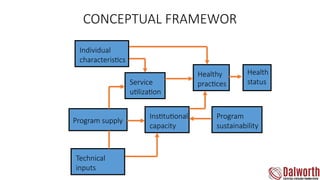
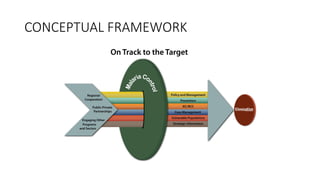
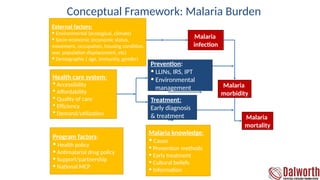
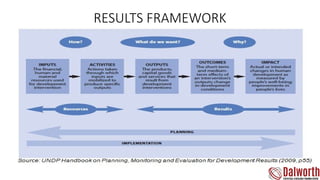
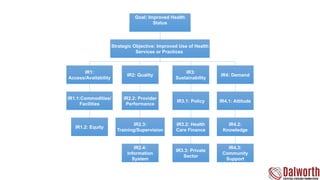
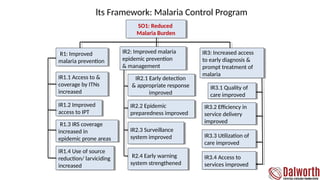
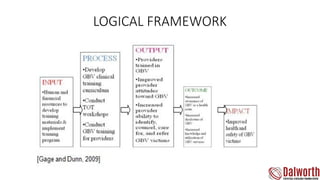
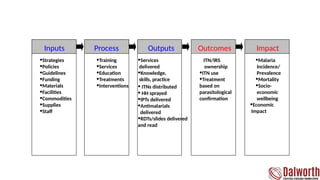
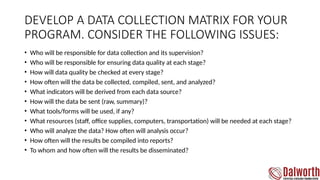
The document outlines a comprehensive results framework for a malaria control program focusing on improving health status and access to health services. It details strategic objectives, indicators for measuring success, and program factors impacting malaria management, including individual characteristics and external influences. Additionally, it emphasizes the importance of a data collection matrix for ensuring data quality and effective reporting.