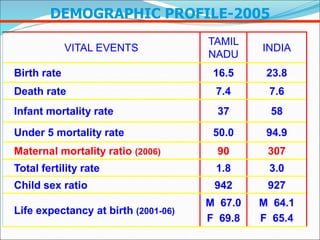
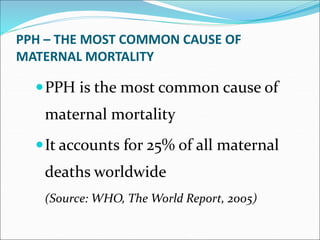
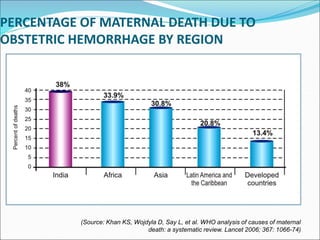
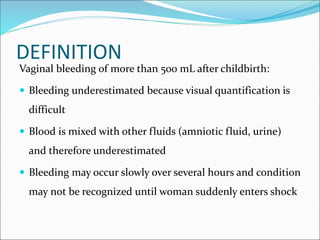
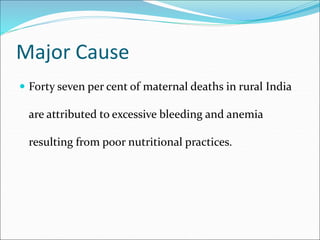
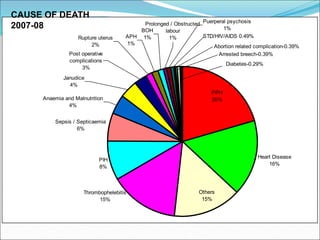
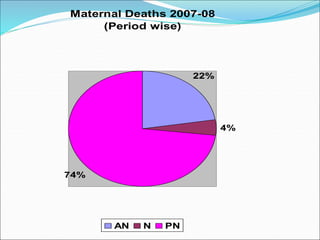
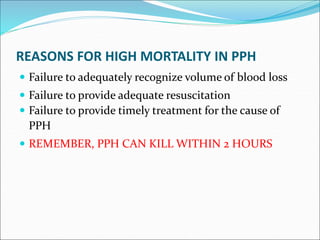
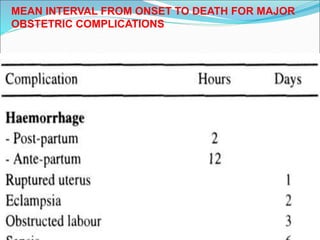
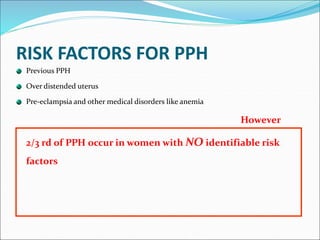
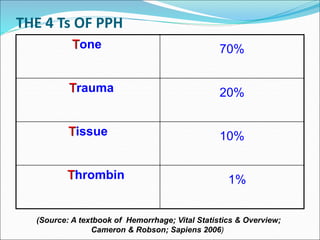
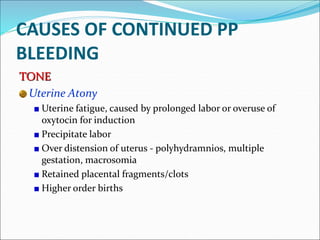
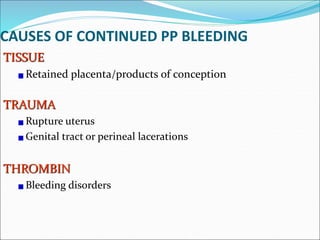
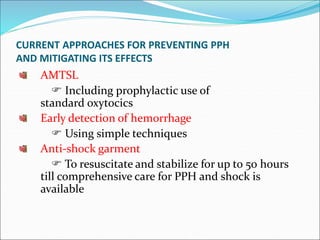
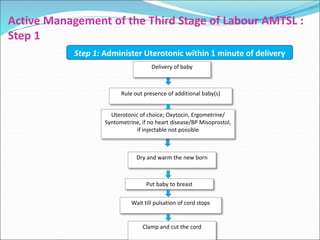
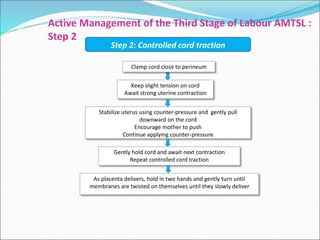
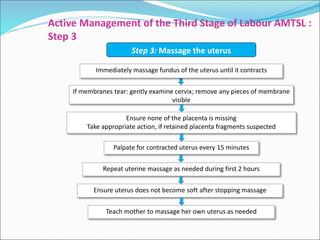
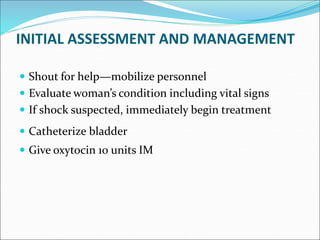
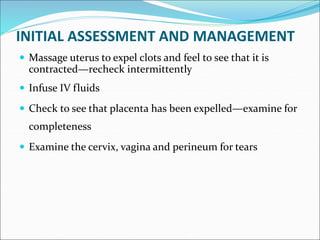
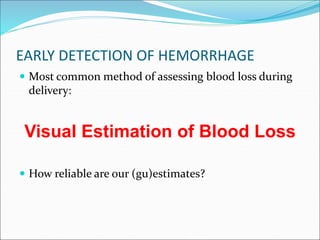
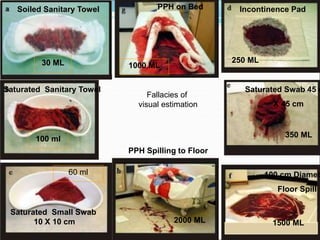
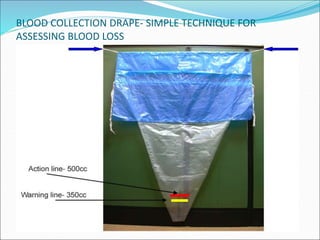
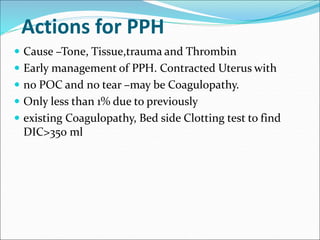
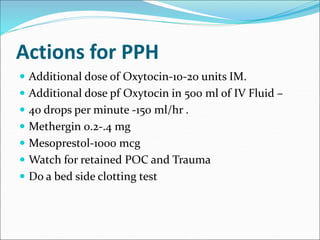
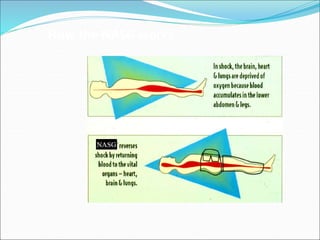
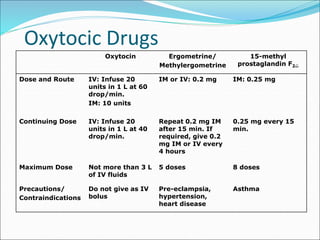
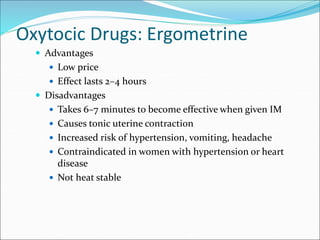
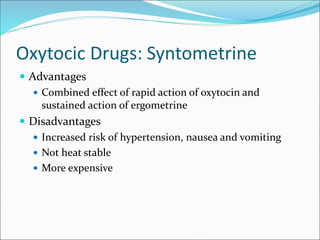
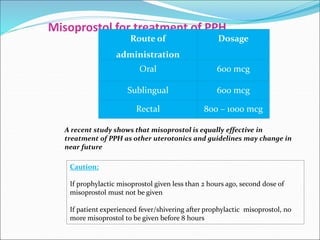
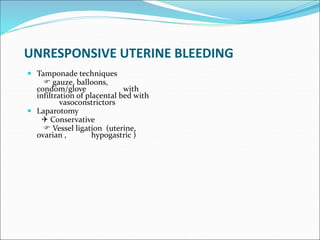
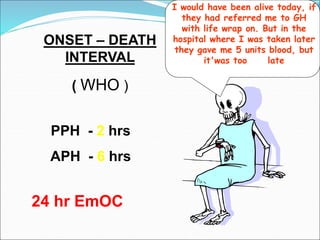
The document discusses critical statistics regarding maternal health in Tamil Nadu, India, emphasizing the high rates of maternal mortality primarily caused by postpartum hemorrhage (PPH). It outlines the causes, management strategies, and the importance of timely intervention in treating PPH. Effective approaches include the administration of uterotonics and active management of the third stage of labor to reduce the risks associated with maternal death.