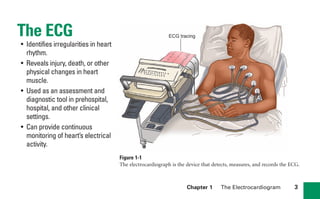
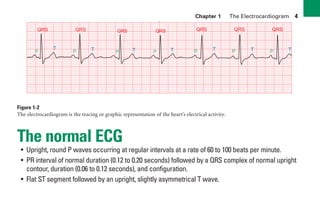
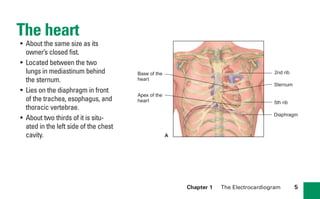
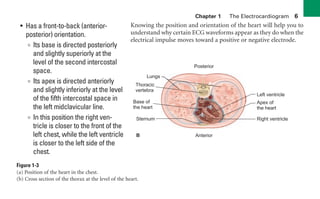
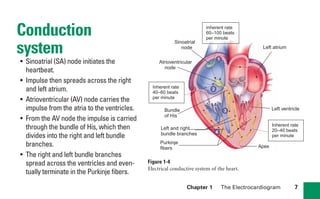
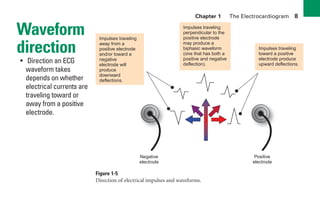
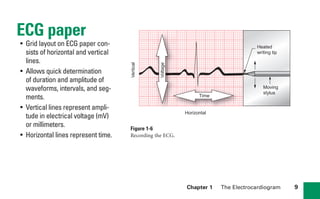
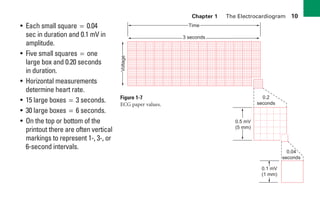
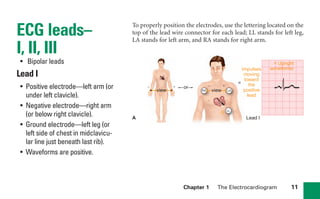
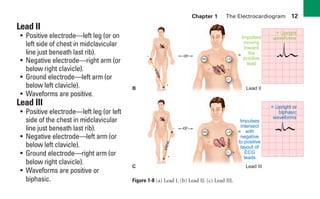
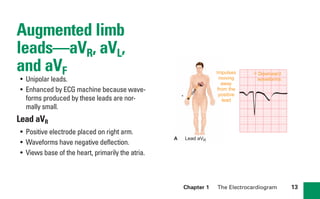
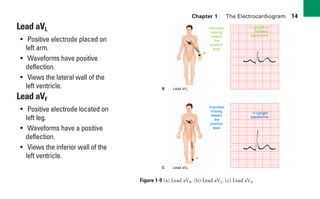
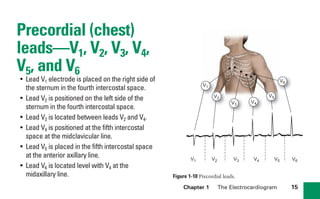
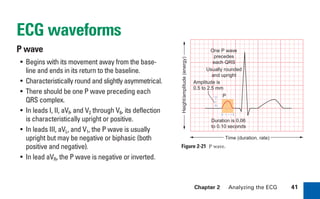
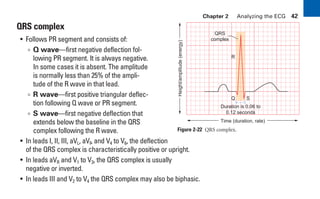
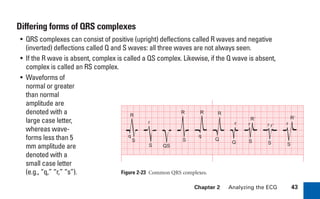
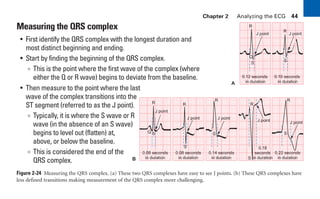
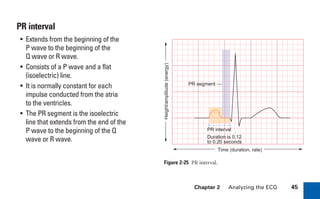
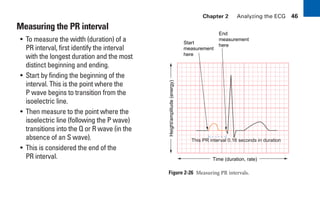
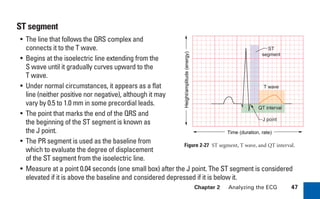
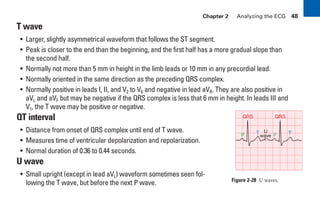
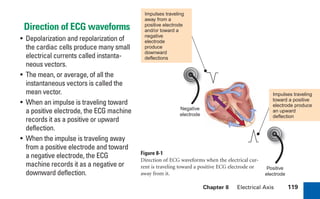
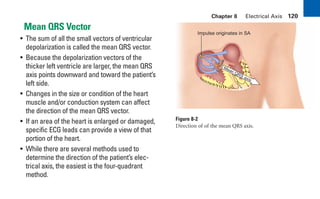
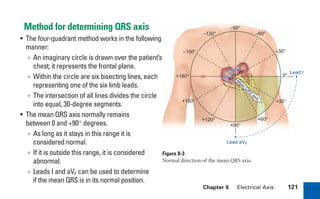
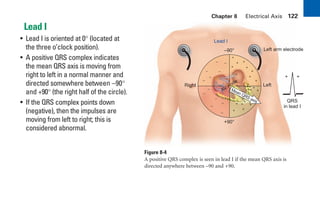
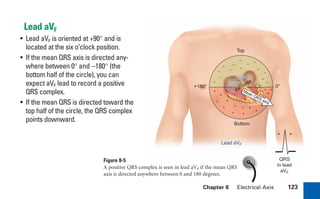
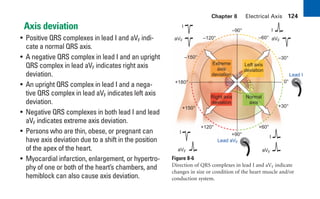
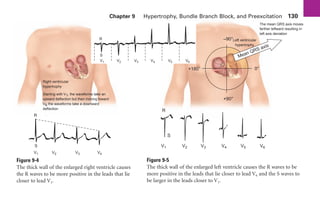
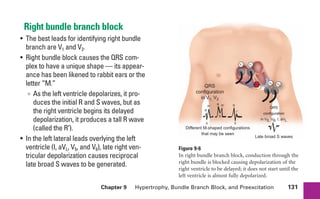
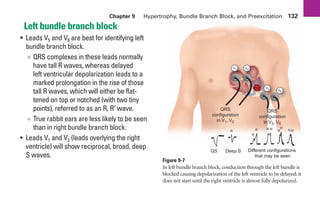
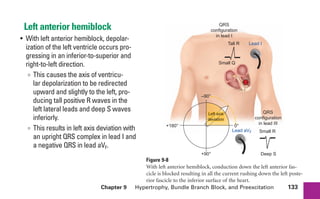
This document provides an overview of electrocardiograms (ECGs) and the heart. It discusses the normal ECG tracing and the heart's electrical conduction system. It describes the standard 12-lead ECG configuration, including limb leads I, II, III and augmented leads aVR, aVL, aVF as well as precordial chest leads V1-V6. It also discusses ECG paper format and how the direction of waveforms is determined by the movement of electrical impulses toward or away from positive electrodes.