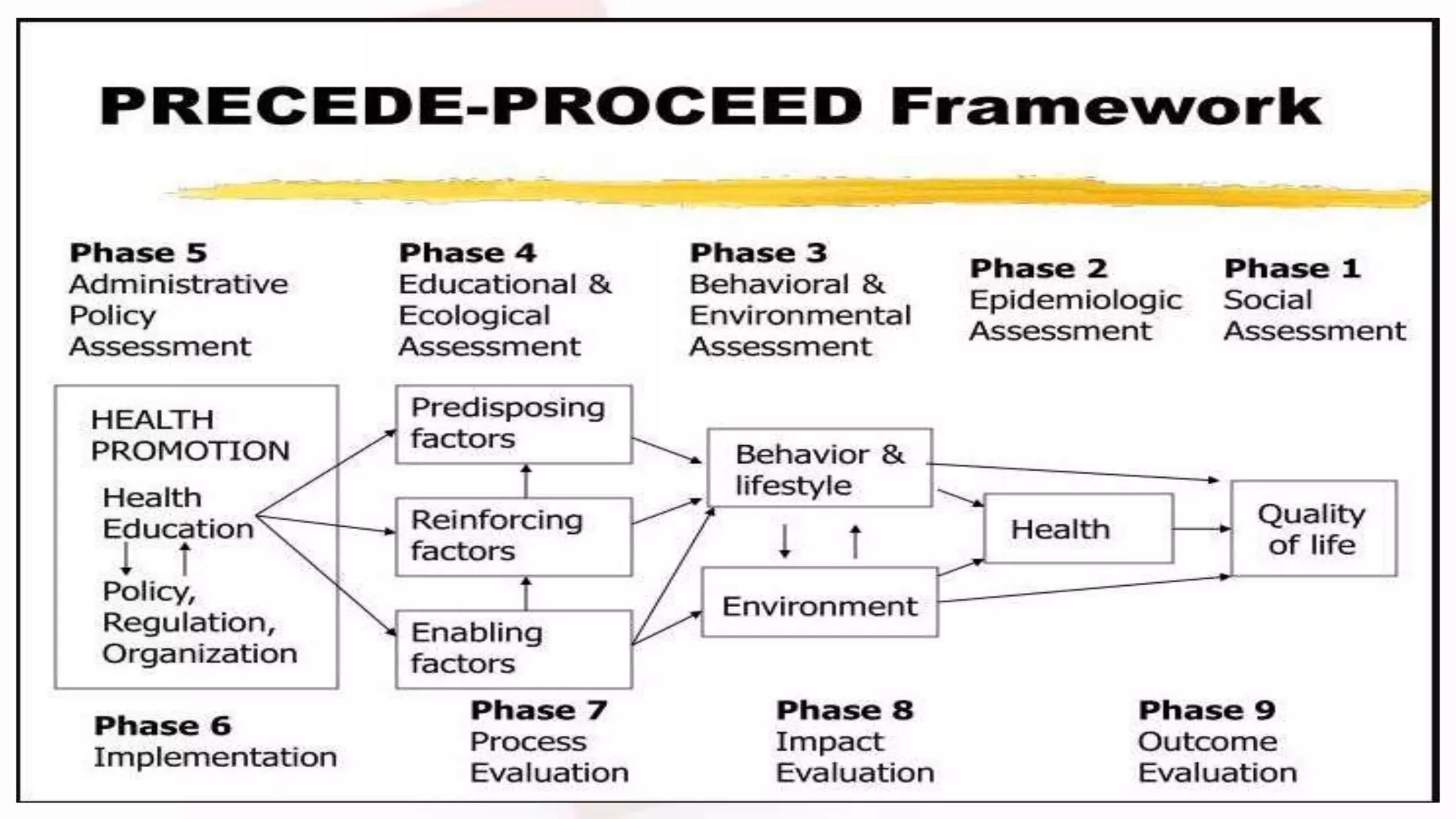
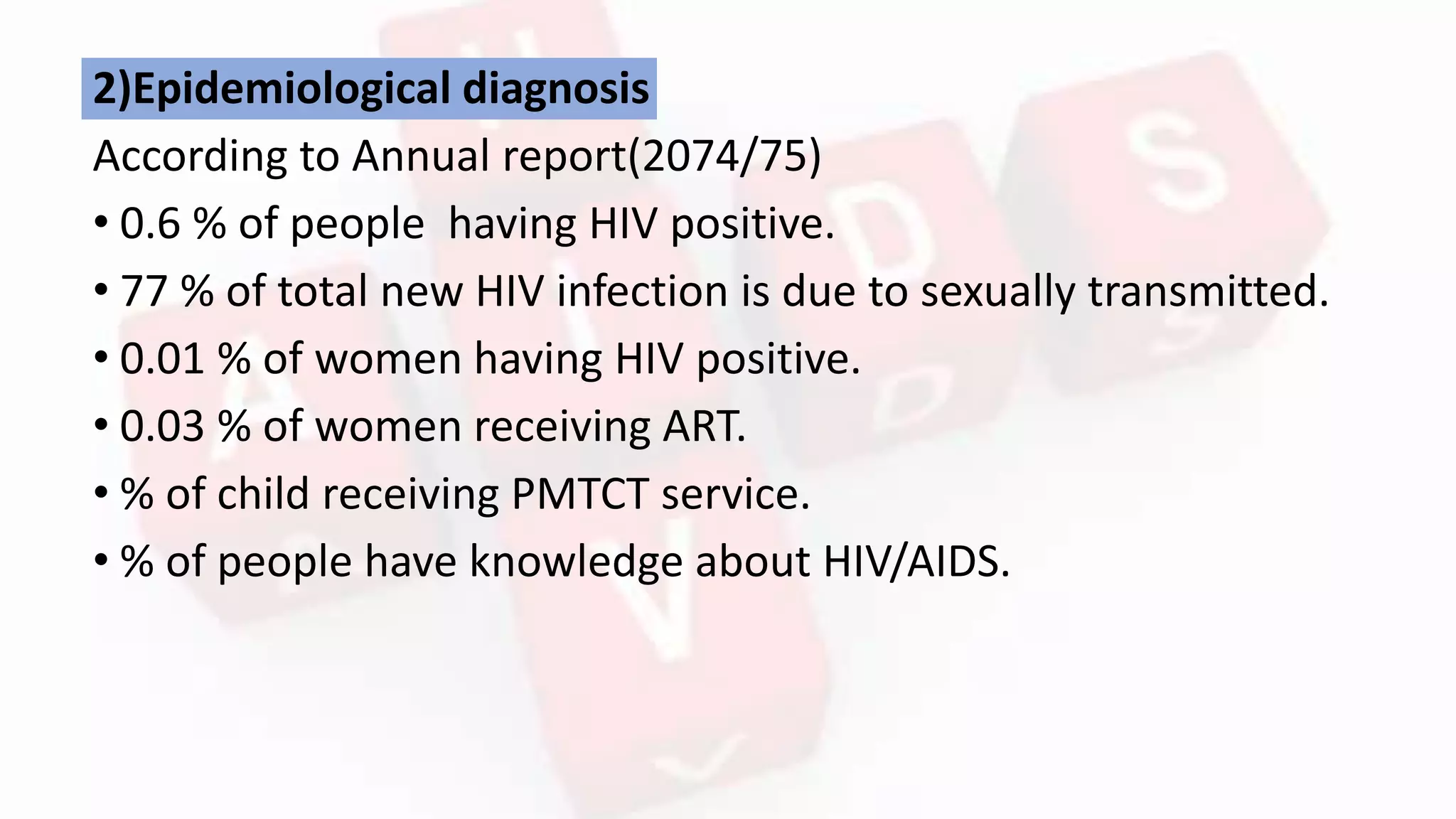
1) The document outlines a plan for an education program on HIV/AIDS in Nepal. It includes an introduction to HIV/AIDS, problem statement on prevalence in Nepal, objectives to reduce transmission and stigma through education, and an evaluation plan.
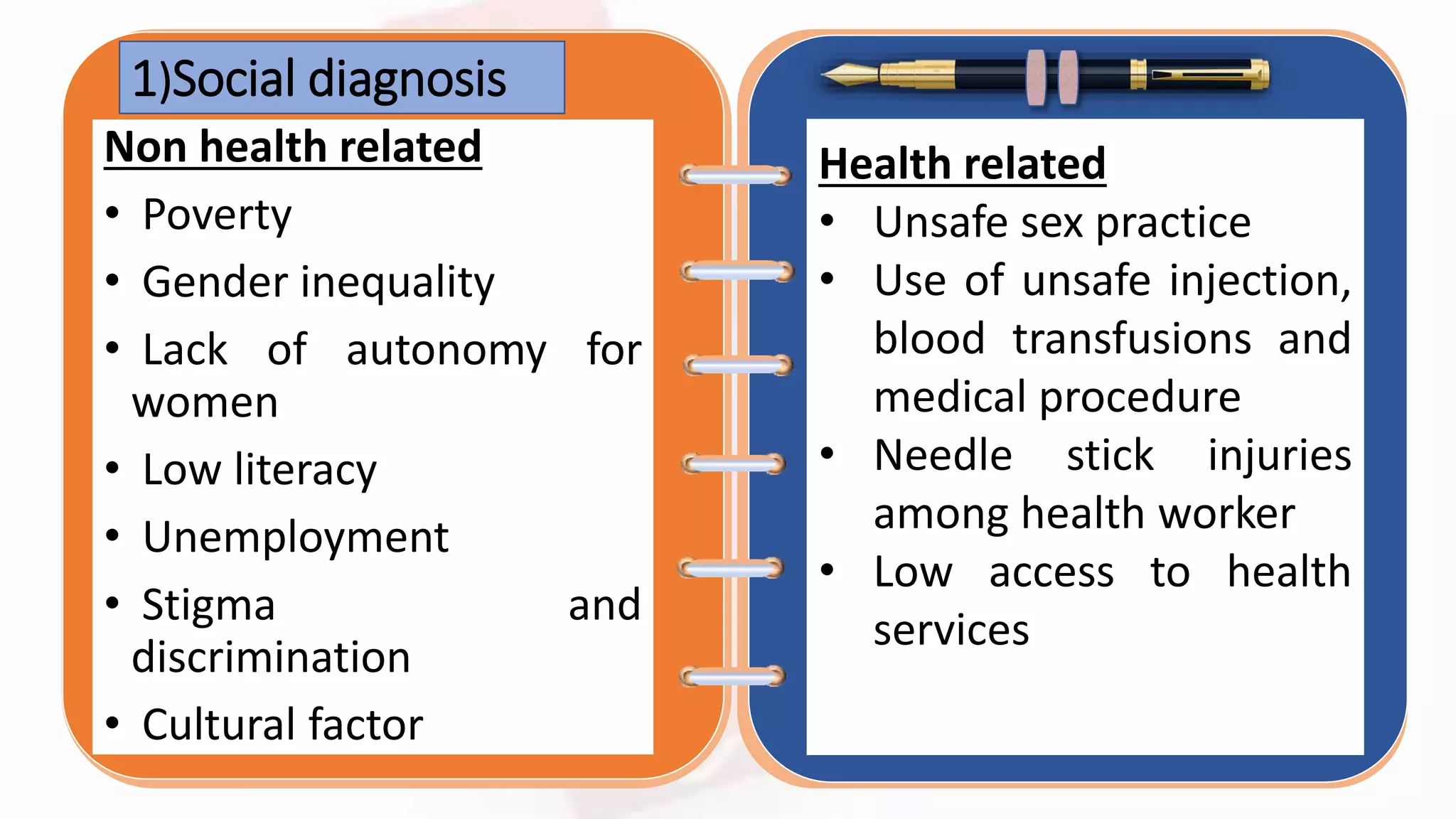
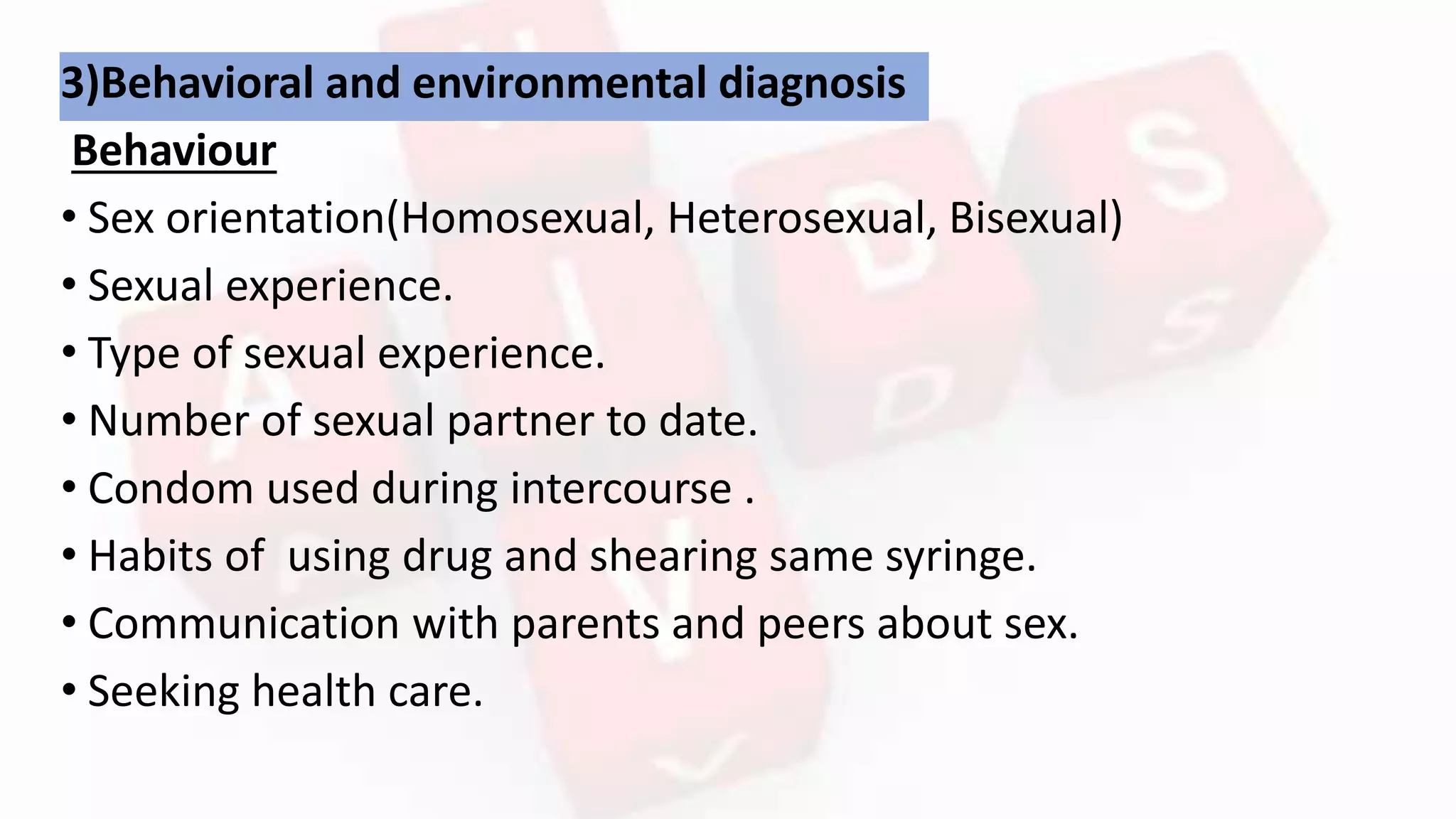
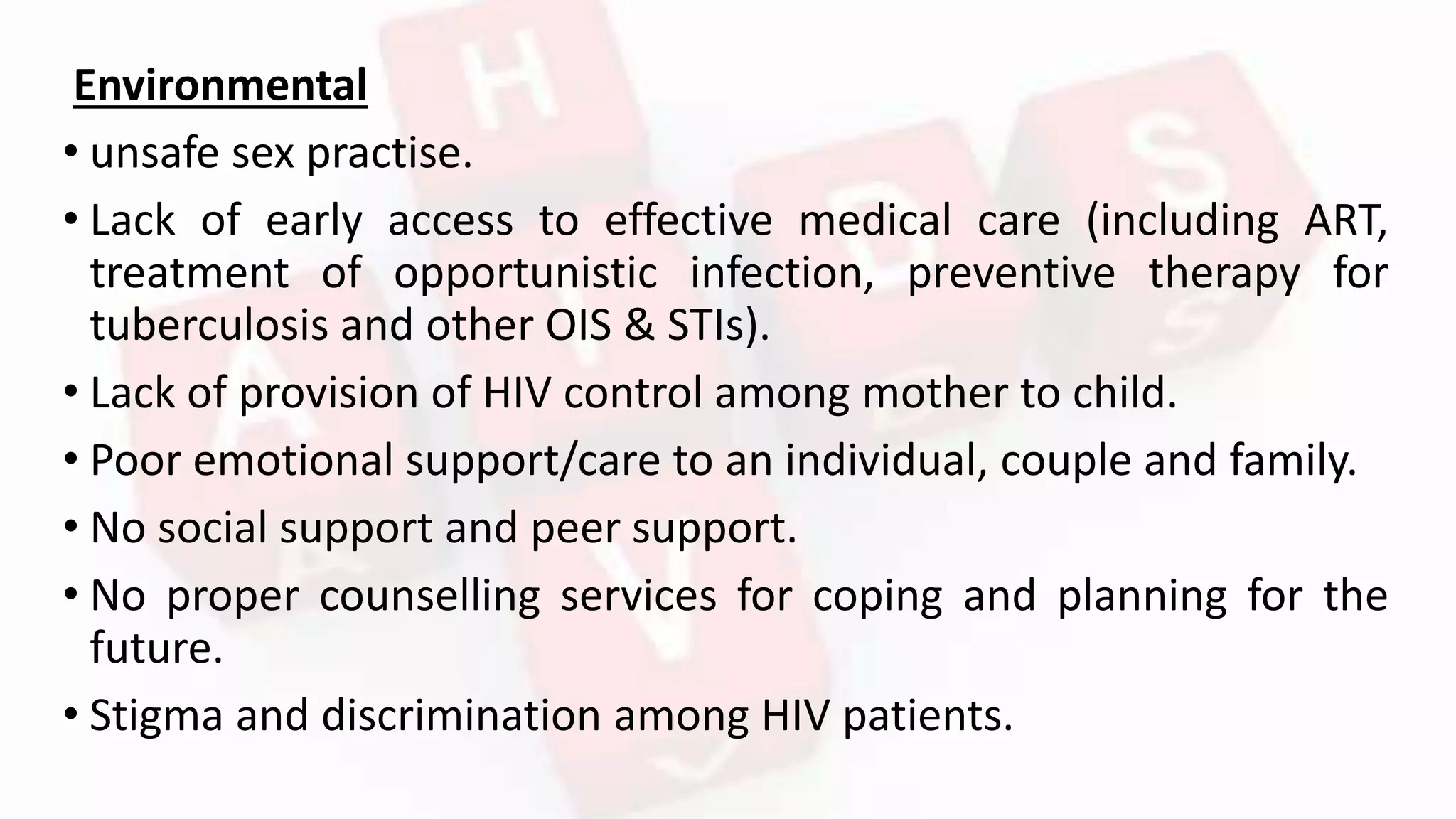
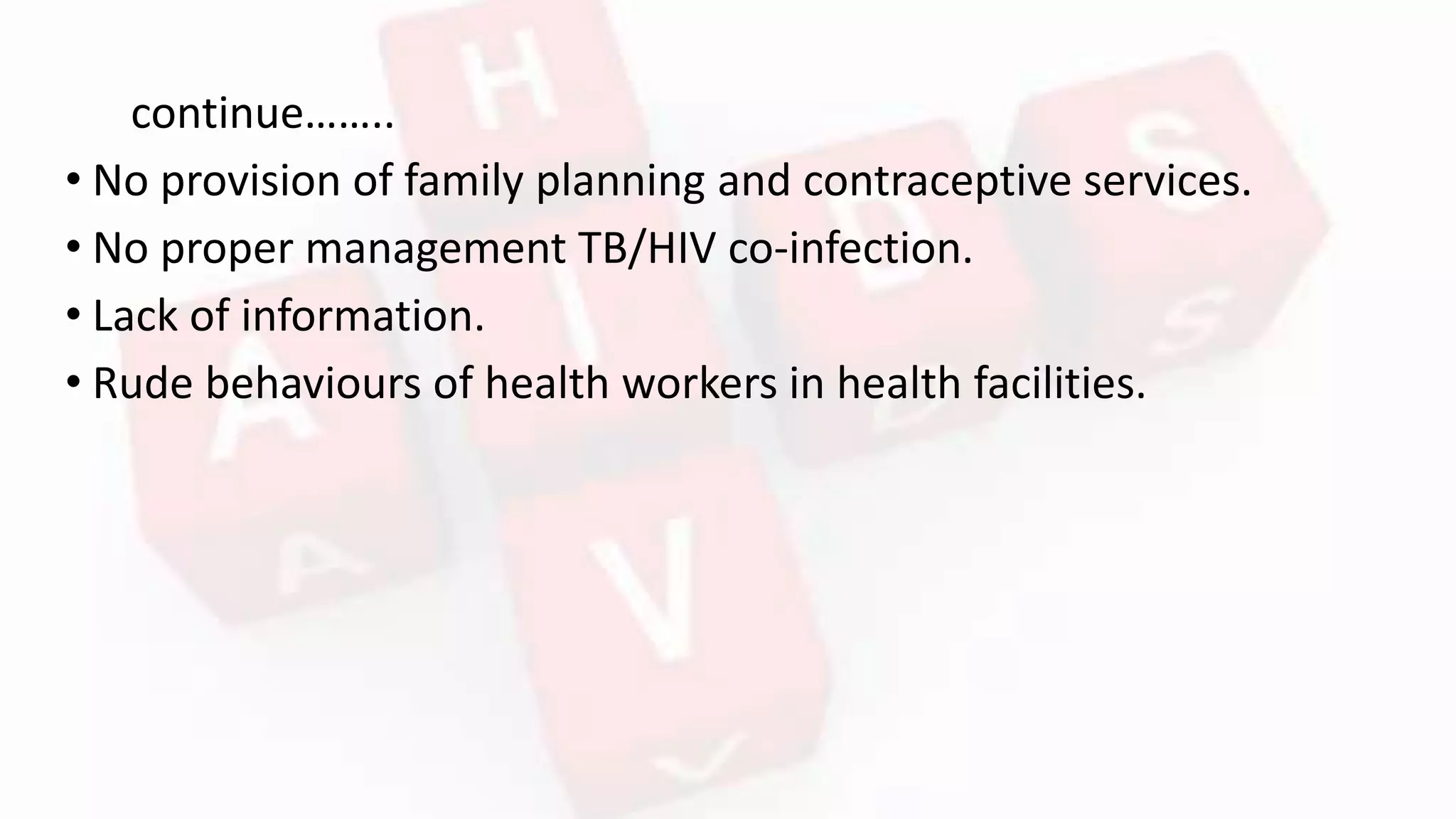
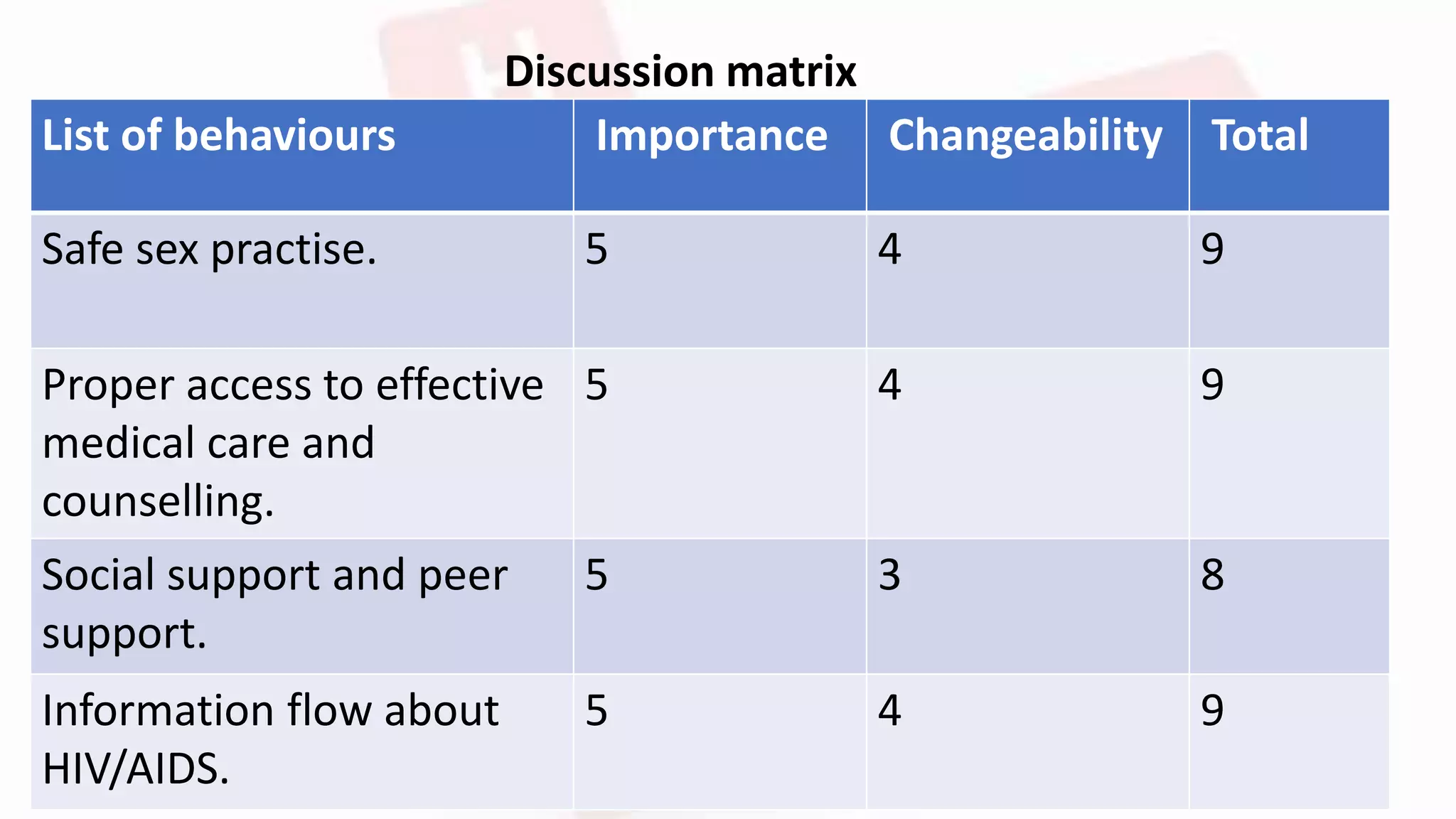
2) A needs assessment identifies risk factors like unsafe sex, lack of access to healthcare, and stigma. The program's goals are to reduce infection rates, increase access to treatment, and coordinate national response.
3) The education program will provide information on transmission, prevention, treatment services, and address stigma through activities like discussion, counseling, and role-playing with targets like key populations and the community.