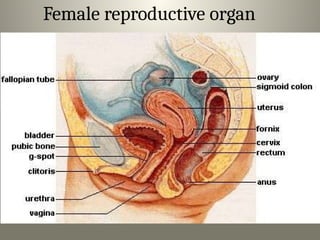
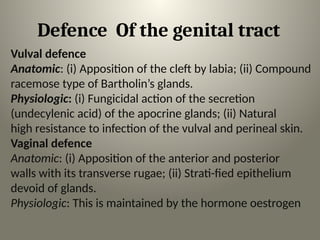
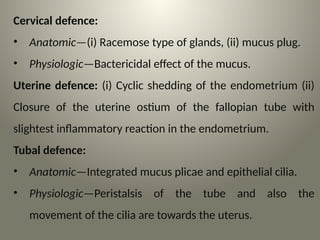
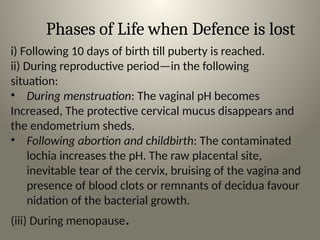
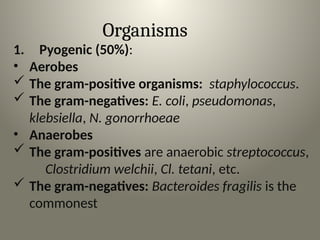
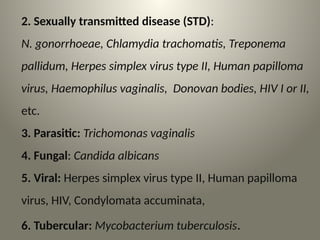
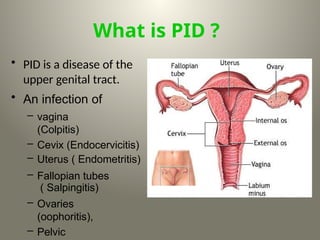
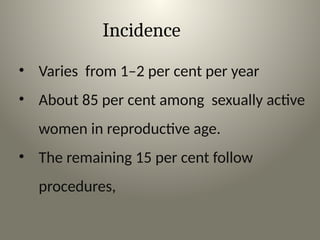
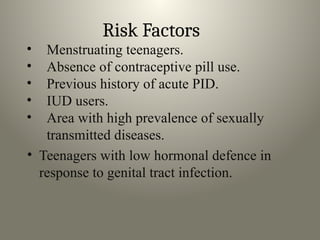
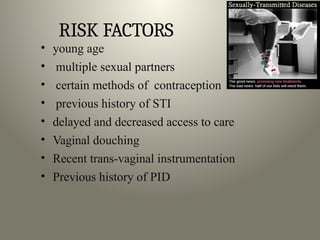
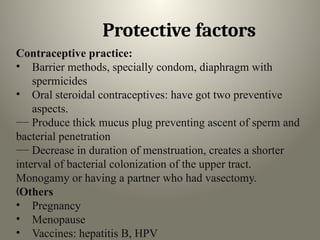
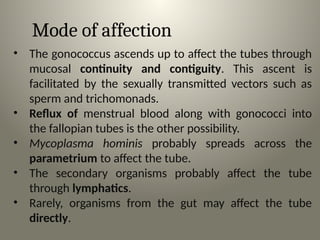
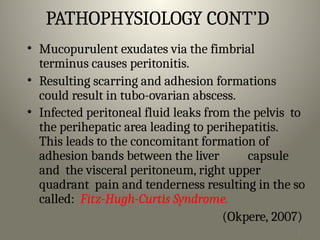
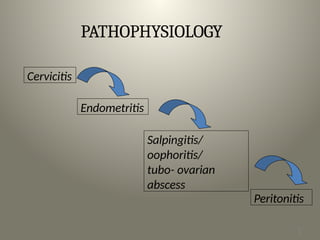
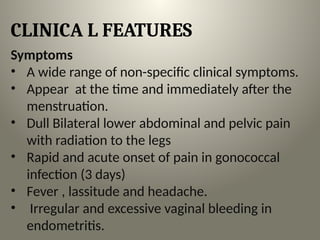
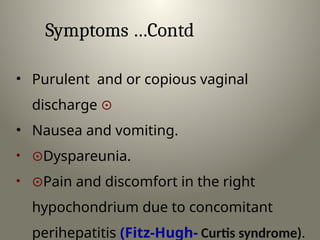
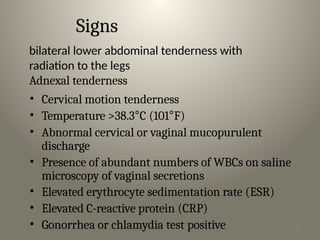
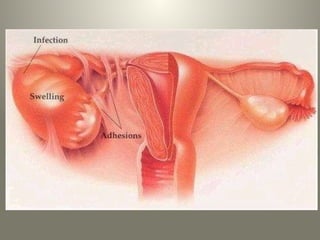
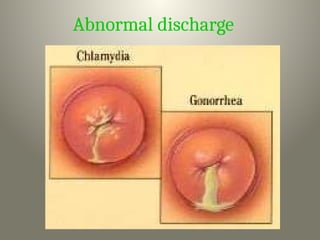
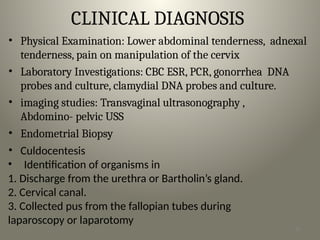
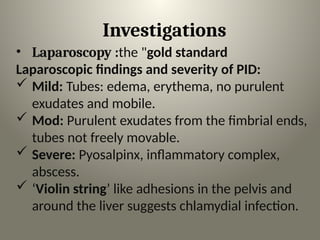
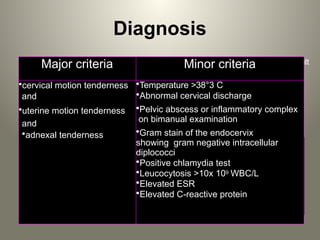
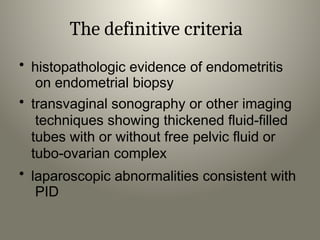
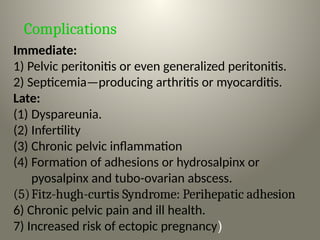
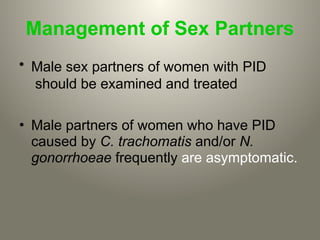
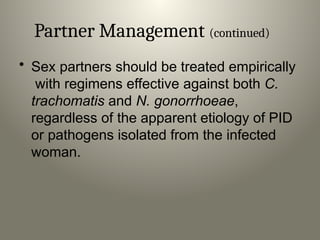
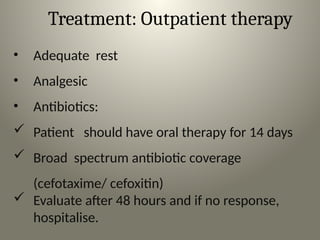
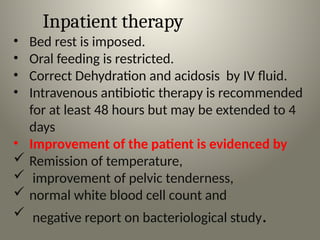
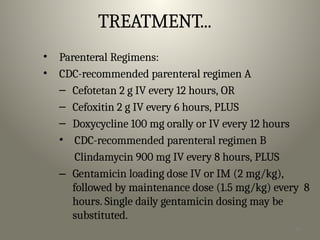
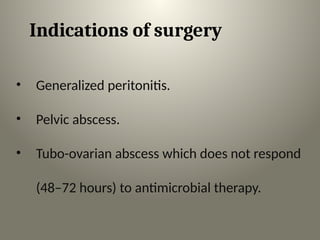
This document outlines pelvic infections, particularly pelvic inflammatory disease (PID), detailing its causes, risk factors, clinical features, and treatment options. It highlights the anatomical and physiological defenses of the female reproductive system, the modes of infection spread, and associated complications. Prevention and management strategies emphasize the importance of safe sexual practices and prompt medical care for affected individuals.