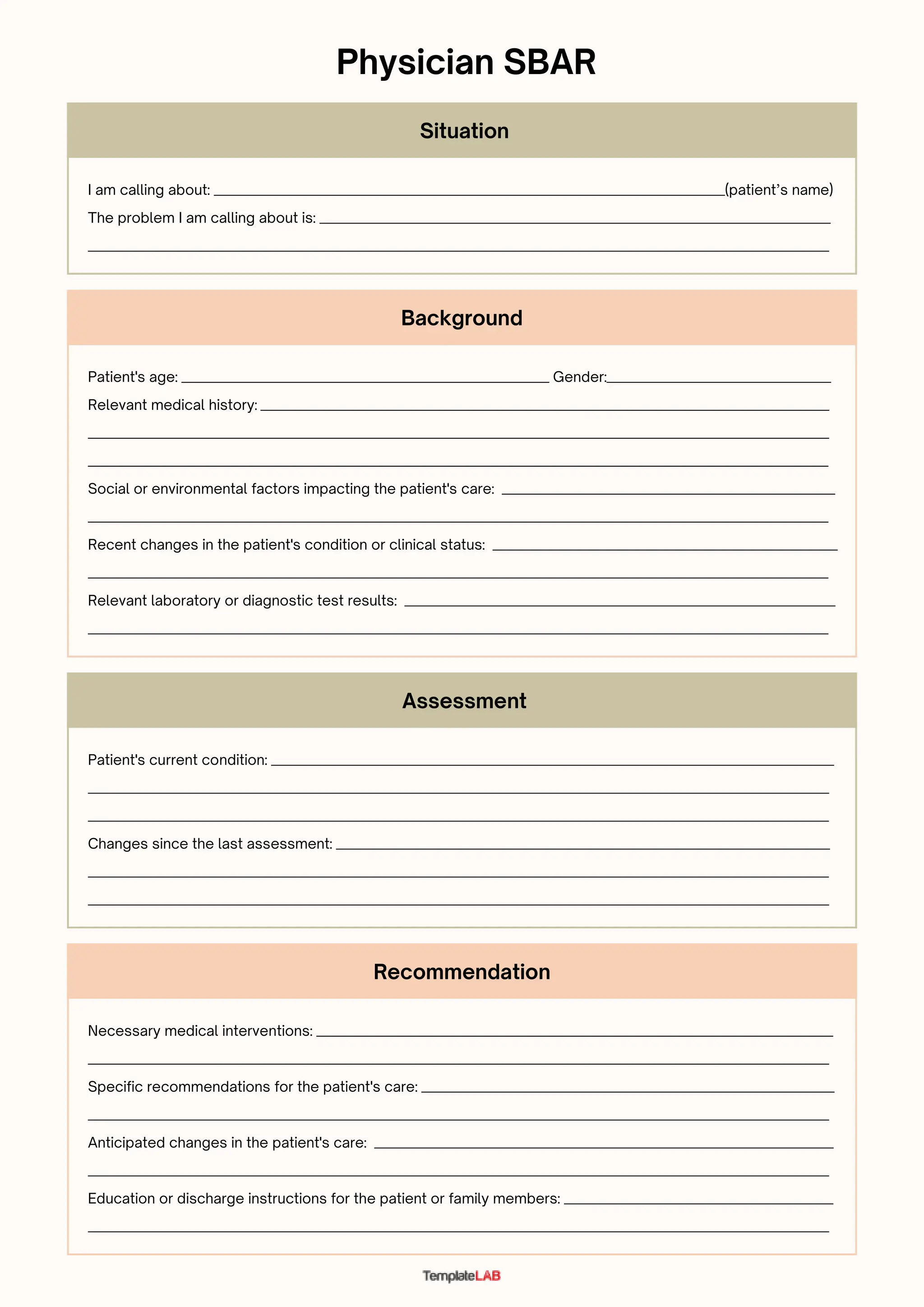
The document provides background information on a patient including their age, gender, medical history, social factors, and recent changes in condition. It also includes a physician SBAR (Situation-Background-Assessment-Recommendation) form which notes the problem being called about, the patient's current condition and any changes, recommendations for necessary interventions and care, anticipated changes, and education or discharge instructions.