The document summarizes the contributions of several physicians who helped advance medicine and public health:
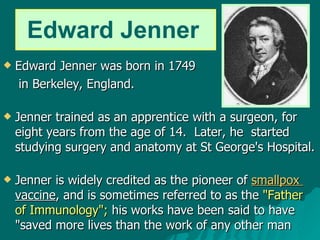
- Edward Jenner developed the smallpox vaccine in 1796 which was pivotal in eradicating the disease.
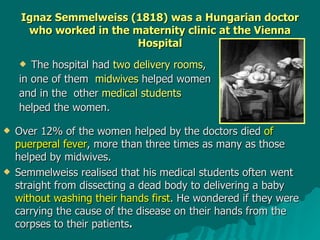
- Ignaz Semmelweis discovered in 1847 that handwashing reduced maternal mortality from puerperal fever in hospitals.
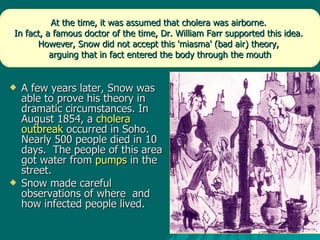
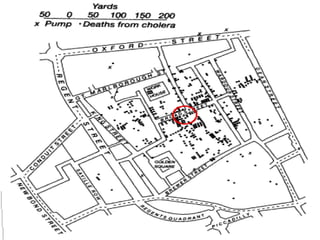
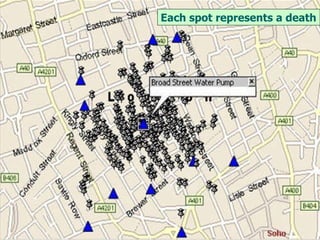
- John Snow conclusively linked a cholera outbreak in 1854 to a contaminated water pump, helping establish germ theory and epidemiology.
- Joseph Lister introduced antiseptic surgery in 1867, reducing surgical infections through carbolic acid and dressings.
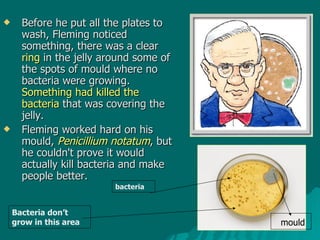
- Alexander Fleming discovered penicillin in 1928 after noticing bacteria-killing mould in his lab, though it