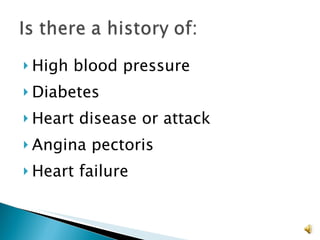
When interviewing patients, establishing trust is essential. Taking a thorough medical history allows clinicians to accurately assess risks and determine if treatment modifications are needed. The initial exam includes checking vitals, conducting a physical exam of major organ systems and the skin, and testing eye acuity to inform the diagnosis and treatment plan.