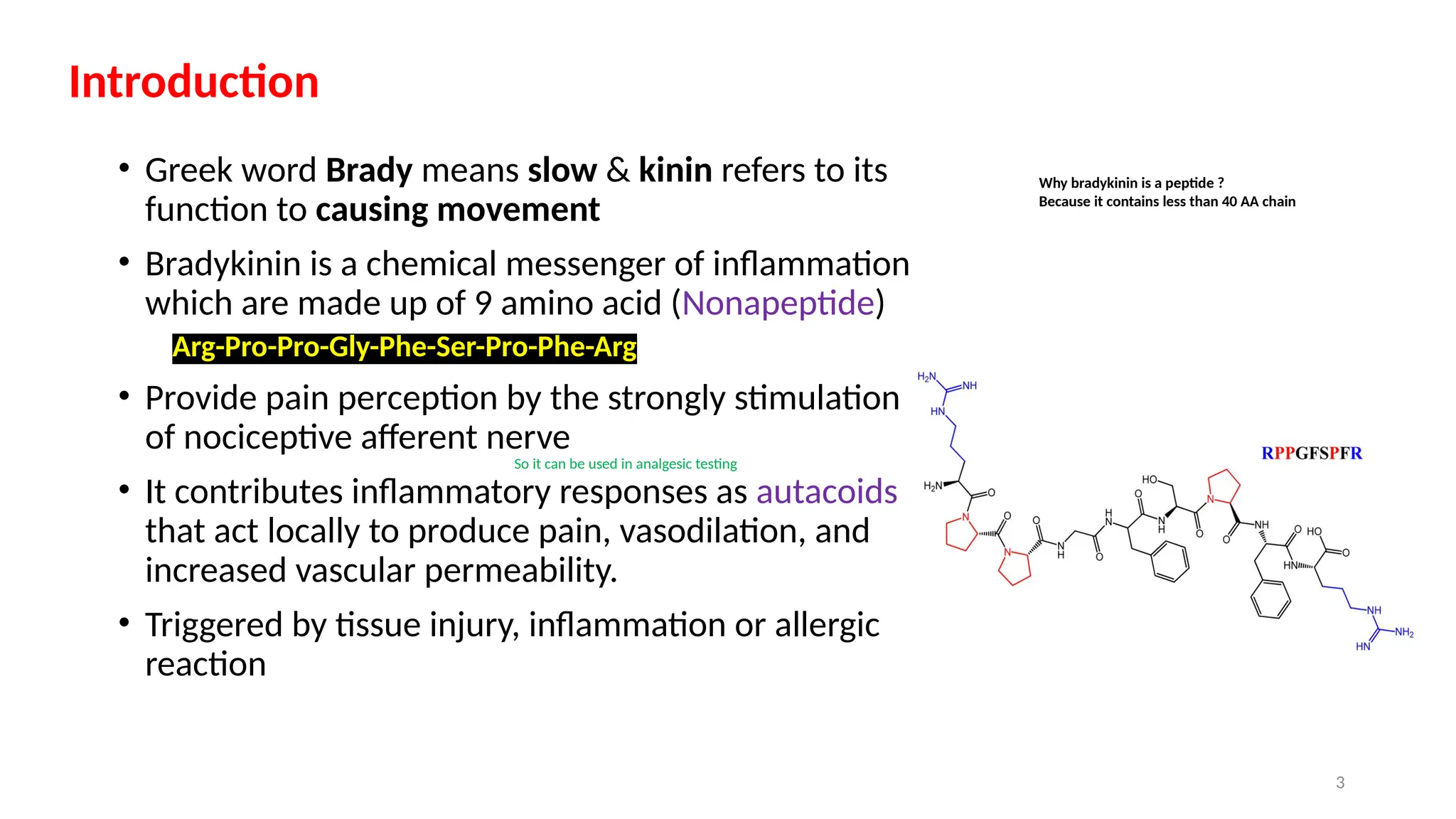
bradykinin is a peptide that is made up of 9 amino acid so it is also called as nonapeptide.
it is a autocoids which synthesis when any injury occur .
it is synthesis by the plasma kallikrein and tissue kallikrein .
it involved in the inflammation and strongly stimulate the nociceptive afferent nerves