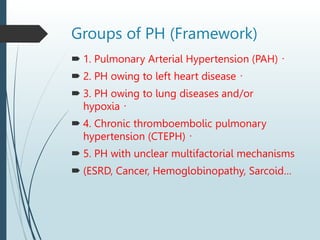
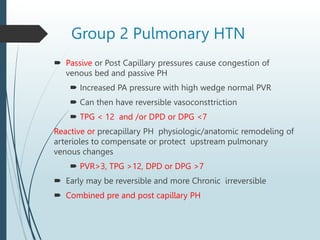
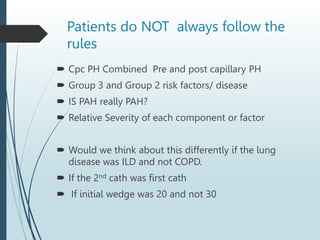
This document discusses a case study of a patient with complex cardiopulmonary issues. The patient presented with COPD exacerbation and was found to have pulmonary hypertension. Initial right heart catheterization found severely elevated pulmonary pressures and pulmonary vascular resistance. After treatment with diuresis and initiation of CPAP, a second catheterization found improved pressures. The document analyzes whether the patient's condition represents pulmonary arterial hypertension alone or a combination of pre-capillary and post-capillary pulmonary hypertension based on the various comorbidities and hemodynamic data. It also discusses challenges in categorizing patients who do not neatly fit classification criteria.