local drug delivery in periodontics
- 2. Contents • Introduction • Systemic antibiotics vs. local drug delivery • Principle of local drug delivery • Goal of local drug delivery • Ideal requirements • Indications, Contra-indications • Advantages, Disadvantages • Classification • Different physical forms • Factors affecting local drug delivery in periodontal pocket 2
- 3. • Non sustained pocket delivery • Sustained release drug delivery. • Controlled release delivery agents • Commonly used drugs LDD •Other Drugs • Future trends • Conclusion 3
- 4. INTRODUCTION • Periodontal disease is a multifactorial disease where putative periodontopathogens trigger chronic inflammatory and immune responses •Usually the host response resolves the infection without pathosis , but if the host- parasite equilibrium is lost, it results in destruction of the tissues (Rabbani GM,Ash MM, Caffesse RG .The effectiveness of subgingival scaling and root plaining in calculus removal. J Periodontal 1981;Volume 52;Number 3.119- 123) • Mechanical therapy has always been the first line of therapy 4
- 5. LIMITATIONS OF MECHANICAL THERAPY • Intra-oral translocation of perio-pathogens. • Invasion into tissues from other intraoral niches such as the tongue, tonsils, and the mucous membranes. • Invasion into dentinal tubules • Bacterial regrowth and recolonization of the pocket occur, with subgingival bacterial counts being restored almost to pre-treatment values 3 to 7 days after treatment Harper DS, Robinson PJ. Correlation of histometric, microbial, and clinical indicators of periodontal disease status before and after root planning. J Clin Periodontol 1987; 14:190-196 Quirynen M, De Soete M, Dierickx K, van Steenberghe D: The intra-oral translocation of periodontopathogens jeopardises the outcome of periodontal therapy. A review of the literature. J Clin Periodontol 2001; 28: 499-507. 5
- 6. Systemic antimicrobial therapy was advocated as an adjunct with mechanical treatment to prevent recolonization of bacteria Greenstein G, Polson A. The role of local drug delivery in the management of periodontal diseases: A comprehensive review. J Periodontol 1998;69: 507-520 SYSTEMIC ANTIBIOTICS IN PERIODONTAL THERAPY Side effects including hypersensitivity, gastrointestinal intolerance and the development of bacterial resistance have been described. Some studies also reported poor results due to -inadequate concentration at the site of action -inability to be retained locally for a sufficient period of time. Goodson JM. Antimicrobial strategies for treatment of periodontal diseases. Periodontol 2000.1994;5:142-68 Walker CB. The acquisition of antibiotic resistance in the periodontal flora. Periodontol 2000.1996;10:78-88. 6
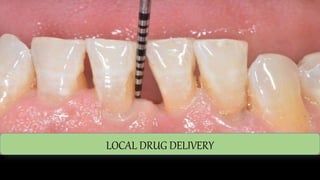
- 7. LOCAL DRUG DELIVERY • To overcome the undesirable effects, several local drug delivery systems have been developed. - It was first proposed by Goodson et al in 1979. He used tetracycline in hollow fibres Goodson J.M.,Haffajee A.,S. S. Socransky:Periodontal therapy by local delivery of tetracycline J Clin Periodontol 1979; 6: 83-92 7
- 8. Stoller et al (1998) studied doxycycline hyclate GOODSON et al 1979 - used hollow tetracycline fibres D. Steinberg et al (1990) researched chlorhexidine as a LDD Nakagawa T et al (1991) used minocycline Ainamo et al (1992) studied 25% metronidazole gel HISTORY 8
- 9. Systemic vs local ISSUE SYSTEMIC LOCAL Drug distribution Wide distribution Narrow effect range Drug concentration Variable levels in different body components high dose at treated sites low levels elsewhere Therapeutic potential May reach widely distribution is better May act better locally on biofilm bacteria Problems Systemic side effects reinfection at the treated sites Diagnostic problems Identification of pathogens , choice of drug Distribution pattern of pathogens and lesions , identification of sites to be treated. Lindhe 4th edition , the use of antibiotics in periodontal therapy; 496-498 ) 9
- 10. Lindhe 4th edition , the use of antibiotics in periodontal therapy; 496-498 10
- 11. TERMINOLOGY LOCAL DRUG DELIVERY/ SITE-SPECIFIC DELIVERY • The terms "local delivery" and "site-specific delivery" are sometimes used synonymously. • A local delivery device consists of a drug reservoir and a limiting element that controls the rate of medicament release. Position paper: The role of controlled drug delivery for periodontitis. J Periodontol 2000; 71:125-140. Sachin Sinha Role of local drug delivery in periodontics: A review.Journal of Research and Advancement in Dentistry July- Oct 2012, Vol.1 No. 3, 11
- 12. DELIVERY SYSTEMS Controlled delivery systems Sustained release 1. less than 24 hours. 2. 2 to 4 applications. 3. may last weeks to months. 4. commonly referred to as sustained-release, prolonged- release, slow release, sustained- action, prolonged-action or extended-action. 1. exceeds 1 day 2. may need to be administered only once. 3. Follow zero order kinetics. 4. commonly referred to as timed-release, controlled- release 12
- 13. First order and zero order kinetics www.pharmainfo.net/og/rcp/downloads 13
- 14. SCIENTIFIC RATIONALE • The scientific rationale for local drug delivery in periodontal pockets was to kill and inhibit the sub gingival bacteria that are not accessible or eliminated by hand or power driven instruments [ Aubrey Soskolni W. Sub gingival delivery of therapeutic agents in the treatment of periodontal diseases. Crit. Res. Oral Bio Med1997; 8(2):164-174]. 14
- 15. GOAL OF LOCAL DRUG DELIVERY The primary goal in using an intra pocket device for the delivery of an antibacterial agent is the achievement and maintenance of therapeutic levels of the drug for the required period of time. This inhibits or kills the pathogens, without any harm to the tissues. [Goodson JM. Controlled drug delivery:A new means of treatment of dental diseases. Compend Cont Educ Dent 1985;6:27-36] 15
- 16. PRINCIPLE SITE FOR LOCAL DRUG DELIVERY The Periodontal Pocket 1. Natural reservoir 2. Easily accessible for insertion of devices 3. GCF is a leaching medium or drug release 4. Gets distributed from pocket Thus, the periodontal pocket is a natural site for treatment with local release delivery system. 16 [ Aubrey Soskolni W. Sub gingival delivery of therapeutic agents in the treatment of periodontal diseases. Crit. Res. Oral Bio Med1997; 8(2):164-174].
- 17. Ideal requisites of locally delivered drug specific for periodontal pathogens Drug must show in-vitro activity against the organisms Target dose sufficient to kill the target organism should not have adverse effects Substantivity Prolonged shelf life Biodegradable and Biocompatible Ease of placement Ready to use chairside Should be economical . Slots J, Rams TE. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000 1996; Vol. 10: 139-59. Goodson JM, Hogan PE, Dunham SL. Clinical responses following periodontal treatment by local drug delivery. J Periodontol; 1985 Special Issue: 81 - 87. 17
- 18. INDICATIONS 1. As an adjunct to scaling and root planing 2. Periodontal maintenance therapy and in shallow and residual pockets post successful phase I therapy 3. For whom surgery is contraindicated or those who refuse surgical treatment Rose LF, Mealey BL, Genco RJ, Cohen DW. Periodontics. China: Elsevier Mosby; 2004 Magnusson I, Lindhe J. et al Recolonisation of a subgingival microbiota following scaling in deep pockets. J Clin Periodontal 1984:11;193-207 18
- 19. CONTRAINDICATIONS 1. Therapies other than LDDs should be considered when: • Multiple sites with PD greater than 5 mm exist in the same Quadrant. • The use of LDAs has failed to control periodontitis (e.g. reduction of PD). • Presence of intra-bony defects)American Academy of Periodontology Statement on Local Delivery of Sustained or Controlled Release Antimicrobials as Adjunctive Therapy in the Treatment of Periodontitis.J Periodontal 2006; Volume 77, Number 8 19
- 20. CONTRAINDICATIONS 2. Periodontal patients with known hypersensitivity reaction to any of the antimicrobials for periodontal therapy. 3. In pregnant or lactating patients 4. Patients susceptible to infective endocarditis to avoid the risk of bacteremia. Rose LF, Mealey BL, Genco RJ, Cohen DW. Periodontics. China: Elsevier Mosby; 2004 Magnusson I, Lindhe J. et al Recolonisation of a subgingival microbiota following scaling in deep pockets. J Clin Periodontal 1984:11;193-207 (Divya P.V, K. Nandakumar. Local drug delivery-Periocol in periodontics. Trends Biomater. Artif. Organs. 2006: 19: 7408020
- 21. 1. Attains a 100- fold higher concentration of anti microbial agent in sub-gingival sites 2. Reduces patient dose by over 400 fold thereby reducing chances of drug resistance and side effects caused by systemic antibiotics 3. Small doses can be administered. 4. Maintain contact with the pathogens in the infected site. 5. Can employ broad spectrum antiseptics like CHX which cannot be given systemically. 6. Super-infection and drug resistance are rare. Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000, 1996; 10: 139159. 21 ADVANTAGES
- 22. DISADVANTAGES 1. Patient may not comply to placement of the drug subgingivally. 2. Does not have any effect on adjacent or nearby structures such as tonsils, buccal mucosa etc so may cause chances of re-infection. 3. Time consuming 4. Costly 5. In presence of generalised pockets, other periodontal therapies should be used. 6. Difficulty in placing the device at the base of the pocket. Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000, 1996; 10: 139159. 22
- 23. I. Langer and Peppas (1981) - Based on their mechanism of action II. Kornman (1993) - Reservoirs with/without a Rate Controlling System III. Rams And Slots, 1996 - Based On application of Therapy IV. Soskolne WA, 1997 - Based on Dosage Form V. Greenstein & Tonetti, 2000 - Based On Duration of Action VI. Soskolone WA , 2004 - Biodegradable devices , Non-degradable devices 23 CLASSIFICATIONS
- 24. CLASSIFICATIONS I. Langer and Peppas (1981) Classified controlled drug release polymeric systems based on their mechanism of action.. 1. Diffusion Controlled Systems a) Matrices (monolithic devices b) Reservoirs (membrane devices) 2. Chemically Controlled Systems a) Erodible systems (biodegradable) b) Pendant chain systems 3. Solvent Activated Systems a) Osmotic systems b) Swelling controlled systems 4. Release Induced By External Forces (magnetic) Langer R, Peppas N. Present and future applications of biomaterials in controlled drug delivery systems. Biomaterials 1981; 2: 201-214. 24
- 25. II. Kornman (1993) has Classified the Controlled Release Local Delivery System as 1. Reservoirs without a Rate Controlling System like hollow fibers, gels and dialysis tubing. (hollow fibres, dialysis tubing, gel) 2. Reservoirs with a Rate Controlling System like Erodible Polymeric matrices, Microporous polymer membrane, Monolithic matrices and coated drug particles.(monolithic fibres, acrylic strips, ethyl cellulose strips,EVA fibres) Kornman KS. Controlled-Release Local Delivery Antimicrobials in Periodontics: Prospects for the Future. J Periodontol. 1993; 64: 782-791. 25
- 26. III. Rams And Slots, 1996: Based On application of Therapy 1) Personally Applied (patient home self-care) A. Non-sustained subgingival drug delivery (home oral irrigation) B. Sustained subgingival drug delivery (none developed to date) 2) Professionally Applied (in dental office) A. Non-sustained subgingival drug delivery (professional pocket irrigation) B. Sustained subgingival drug delivery (controlled release device) Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pockets. Periodontology 2000 1996;10:139-159. 26
- 27. IV. Soskolne WA, 1997: Based on Dosage form Devices have been developed in three broad dosage forms: a. Fibers e.g. Tetracycline b. Films/ slabs e.g. Chlorhexidine chip 1. Non-degradable films 2. Degradable devices c. Injectable systems e.g. Minocycline Soskolne WA, Heasman PA, Stabholz A, et al. Sustained local delivery of Chlorhexidine in the treatment of Periodontitis: a multicenter study. J Periodontol 1997;68:32-38. 27
- 28. V. Greenstein & Tonetti, 2000 Based On Duration of Action According to the duration of drug release, the local delivery devices used in periodontology can be divided into two classes: A. Sustained Release Devices • Drug delivery for less than 24 hrs • Require multiple applications • Follow first order kinetics B. Controlled Release Devices • Duration of drug release exceeds 24 hrs or for atleast 3 days following application e.g. 5% clindamycin in Eudragit Greenstein G, Tonetti M. Academy report: The role of controlled drug delivery for periodontitis (Position paper). J. Periodontol. 2000; 71: 125-140. 28
- 29. VI. Soskolone WA, Friedman M. Intra pocket devices can be divided in two broad categories Depending on degradability: 1. Non-degradable devices (first generation) 2. Biodegradable devices (second generation) Soskolone WA, Friedman M. Intra-periodontal Pocket Drug Delivery Systems. Ed By Michael J Rathbone., In: Oral Mucosal Drug Delivery 2004; 74, Marcel Dekker Inc; 359- 79. 29
- 30. Factors Affecting Local Delivery of Agents in Periodontal Pockets (Goodson 1979) The most important factors that affect the local delivery of agents to the periodontal pocket are 1. Subgingival drug- microbial contact 2. Effective subgingival drug concentration. 3. Time. 4. Substantivity. 30
- 31. Sub-gingival drug microbial contact • An adequate drug-microbial contact time must be attained for an antimicrobial agent to exert its bactericidal or bacteriostatic effects against targeted microorganisms. Gingival crevicular fluid flow into • Periodontal pockets averages 20 чl per hour and markedly increases with tissue inflammation. • Hence, inflammation needs to be controlled prior the use of LDDs. Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pockets. Periodontology 2000 1996;10:139-159. 31
- 32. Effective Subgingival Concentration • Drug should have a dose higher than Minimal Inhibitory Concentration (MIC). • Antimicrobial agents that exert bactericidal effects within a 5-minute time period are preferable for sub- gingival irrigation. Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pockets. Periodontology 2000 1996;10:139-159. 32
- 33. TIME • Once a drug reaches the site of action in an effective concentration, it must remain at the site enough for its pharmacological effect to occur. • Drug kinetics should follow zero order to stay there for long time Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pockets. Periodontology 2000 1996;10:139-159. 33
- 34. SUBSTANTIVITY • Substantivity refers to property of a substance to bind to soft and/ or hard tissue of the pocket, thereby establishing a drug reservoir. • Incorporation of drug into various vehicles or devices, prior to placement into periodontal pocket enhances substantively. Influenced by a series of parameters like: • Concentration of the medication • Length of time of contact of the solution with the oral structures • pH • Temperature Goodson J. Pharmacokinetic principles controlling efficacy of oral therapy. J Dent Res 1989;68: 1625- 32. Greenstein G,Tonetti M.Academy report: The role of controlled drug delivery for periodontitis(Position paper).J Periodontol 2000;71:125-40. 34
- 35. Design of local periodontal delivery systems • Once an intrinsically efficacious drug is selected the design of its local periodontal delivery device requires the definition of several objectives. • As a general rule dosage regimens to treat biofilm based infections aim at obtaining a profile able to maximise the area under the concentration curve; i.e obtaining high concentrations for longer durations. 35
- 36. • The intracrevicular delivery devices should be loaded with a drug reservoir of sufficient size to satisfy the concentration and time objectives. • The same antimicrobial is available in different chemical forms with different solubility profiles; • The selected antibiotic may in itself impose limitations on the choice of carrier (resorbable or non resorbable) 36
- 37. Vehicles • Solutions • Paste • Hollow fibres • Acrylic strips • Monolithic fibres • Resorbable cellulose • Collagen • Biodegradable gel. 37
- 38. INJECTABLE SYSTEMS Easy & effective Cost saving STRIPS & COMPACTS Polymers and monomers impregnated with drug Metronidazol e CHX, Augmentin, Tetracycline, Doxycycline VESICULAR SYSTEMS Mimic biomembra nes Triclosan., CHX MICROPARTI CLE SYSTEM Biodegradabl e PLA or PGLA Tetracycline & doxycycline microspheres NANOPARTIC ULATE SYSTEM Targeted controlled slow drug release Bioadhesive & increases stability FIBRES Hollow Monofilament Tetracycline Chlorhexidine FILMS Matrix delivery systems Biodegradable – Soluble films Fish collagen Dissolution Steinberg et al Non biodegradable – Insoluble films Ethyl cellulose diffusion CHX, tetracyclines, metronidazole GELS Solid/semisoli d formulations Base – Methyl cellulose CHX, metronidazol e, tetracycline etc 38 VARIOUS DELIVERY SYSTEMS USED
- 39. STRIPS & COMPACTS Polymers and monomers impregnated with drug Metronidazole CHX, Augmentin, Tetracycline, Doxycycline VESICULAR SYSTEMS Mimic biomembranes Triclosan., CHX MICROPARTICLE SYSTEM Biodegradable PLA or PGLA Tetracycline & doxycycline microspheres NANOPARTICULATE SYSTEM Targeted controlled slow drug release Bioadhesive & increases stability 39
- 40. COMPARISON OF DRUG DELIVERY SYSTEMS FOR THE MANAGEMENT OF PERIODONTITIS 40
- 41. DRUG SELECTION • Identification of periodontal pathogens • Is advisable to do bacterial culture and sensitivity testing - Magnusson 1989 e.g., Tetracyclines often administered, as they are broad spectrum antibiotics. However studies also showed patients previously treated with tetracycline responded not well and other antibiotics were beneficial • No single drug is the universal drug of choice. 41
- 42. VARIOUS DRUGS/AGENTS USED IN THE LOCAL DRUG DELIVERY SYSTEMS 1. TETRACYCLINE 2. DOXYCYCLINE 3. MINOCYCLINE 4. METRONIDAZOLE 5. CHLORHEXIDINE 6. OTHER DRUGS LIKE CLARITHROMYCIN, ALENDRONATES, OFLOXACIN, CLINDAMYCIN and other newer drug delivery systems. 42
- 43. TETRACYCLINE • Broad spectrum antibiotics with activity against both gram positive and gram negative organisms. • Bacteriostatic agents but may have a bactericidal effects in high concentrations (Walker 1996). These drugs principally acts by inhibiting protein synthesis • Goodson’s first delivery devices involved hollow fibres of cellulose acetate filled with tetracycline in 1979. • Consist of four fused cyclic rings and the various derivatives consist of only minor alterations of the chemical constituents attached to this basic ring structure. • Tetracycline, Doxycycline and Minocycline are commonly used with similar spectrum of activity. Hence resistance to one indicates resistance to all the three 43
- 44. VARIOUS DRUGS USED AS CONTROLLED RELEASED SYSTEMS TETRACYCLINE : • Broad spectrum antibiotics with activity against both gram positive and gram negative organisms • Consist of four fused cyclic rings and the various derivatives consist of only minor alterations of the chemical constituents attached to this basic ring structure 44
- 45. • In addition to its antibacterial action, it also possess the following function: •Demineralizes dentin cementum and dentin, when applied topically •Enhancing attachment of fibroblasts to the tooth surface (Wikesjo et al 1986; Morrison et al 1992) 45
- 46. • Has high substantivity i.e. after local delivery, it has been detected at 1-20µm within epithelial tissues (Ciancio et al 1992) • Detectable in high concentrations GCF several weeks following application (Wikesjo et al 1986) • Collagenase inhibition, anti-bone resorption effect, anti- inflammatory actions 46 ADVANTAGES
- 47. DISADVANTAGES 1. Development of antibiotic resistance 2. Ability to kill benign organisms associated with health as well as pathogens. Lacroix JM, Walker CB. Detection and incidence of the tetracycline resistant determinanttet (m) in the microflora associated with adult periodontitis. J Periodontol 1995;66(2):102 108. 47
- 48. TETRACYCLINE LDD SYSTEMS tetracycline Tetracuycline fibres Tetracycline gel Tetracycline films 48
- 49. 1. TETRACYCLINE GEL The purpose was to reduce the polymer concentration and to obtain reasonable viscosity at a lower concentration of pluronic acid. A 20% wt/wt pluronic gel - Tetracycline Serratiopeptidase Containing Periodontal Gel Formulation 2. TETRACYCLINE FILMS Atelocollagen films with immobilized tetracycline have been found to produce an effective MIC dose in the gingival crevicular fluid for up to 10 days. [M. Minabe, A. Uematsu, K. Nishijima, E. Tomomatsu, T. Tamura,T. Hori, T. Umemoto, T. Hino, Application of a local drug delivery system to periodontal therapy. Development of collagen preparations with immobilized tetracycline, J.Periodontol. 60 (1989) 113± 117 Maheshwari M, Miglani G, Mali A, Paradkar A, Yamamura S, Kadam S. Development of Tetracycline Serratiopeptidase Containing Periodontal Gel: Formulation and Preliminary Clinical Study; AAPS Pharm Sci Tech 2006; 7 (3) Article 76:E162- 171. 49
- 50. SERUM AND GCF CONCENTRATION OF COMMONLY USED ANTIBIOTICS 50
- 51. PERIOCOL TC The first generation non-degradable devices have been replaced by the second-generation degradable devices . • PerioCol -TC vial contains Type1, fibrillar collagen of fish origin of approximately 25 mg, impregnated with approx. 2.0mg of Tetracycline Hydrochloride IP, sterilized by gamma irradiation. - releases tetracycline invitro for a period of 8 to 12 days. - biocompatible and absolutely safe for human applications PerioCol-TC should not be used in any Patient with a known sensitivity to Tetracycline Hydrochloride and Collagen. Not recommended in acutely abscessed periodontal pocket 51
- 52. TYPES OF FIBRES • MONLITHIC • HOLLOW • RESORBABLE 52
- 53. TETRACYCLINE fibres (ACTISITE) • They are non-resorbable cylindrical drug delivery devices made of a biologically inert, plastic co-polymer loaded with 25% tetracycline HCL powder (Goodson et al 1983) • 23 cm in length and 0.5 mm in diameter. The fibre is flexible and can be folded on itself to nearly fill the pocket • Able to release and maintain tetracycline for a period of 7 days (Tonetti et al 1990) with mean concentrations of 43µg/ml in the superficial portions of the pocket wall • At a concentration more than 150 times achieved by systemic tetracycline, these fibres provide bactericidal concentration of tetracycline. 53
- 54. TECHNIQUE • An individual or several teeth can be treated at a time • Short lengths of fibre, 2-3 inches are taken in a cotton forceps and placed at the opening of the pocket to be treated • The fibre folded on itself • The folding procedure might be repeated until all the pockets are nearly filled 54
- 55. • Interproximal pockets should be packed from both the buccal and the lingual sides • After placement, the area is isolated with cotton rolls or gauze, tooth dried with the air syringe and a drop of tissue adhesive applied at each interdental area as well as facially and lingually • Alternatively, periodontal pack can be placed (Goodson et al 1985) • Fibres should be in place for 7-14 days • Fibre removal (in case of non-resorbable fibres) is fairly simple. They can be teased out of the pockets with a curette 55
- 56. . 2-3 inches placed at the opening of the pocket to be treated- isolation is required Folded inside – buccal, lingual, interproximally. DROP OF TISSUE ADHESIVE 7-14 days later , removed with curette PACK can be placed56
- 57. INSTRUCTIONS TO BE GIVEN TO THE PATIENT • Not to brush or floss the treated areas until fibres are removed • To rinse with chlorhexidine mouth rinse while the fibres are in place and for 1 week after their removal • Advised to return back to normal original oral hygiene procedure after 1 week or after fibre removal (in case of non-resorbable fibres) • To come for recall visit at 4-6 weeks 57
- 58. 58
- 59. Review of Literature Goodson et al (1979) showed the virtual elimination of spirochetes from the gingival sulcus is possible by a single placement of tetracycline-filled hollow fibers local Drug Delivery and spirochetes, once eliminated from a site, do not rapidly re-colonise despite the persistence of viable organisms elsewhere in the mouth. Goodson et al (1985) compared the hollow fibres versus monolithic ethyl vinyl acetate. Monolithic fibre loaded with 25% tetracycline provided sustained release for 10 days. The average intrasulcular tetracycline concentration measured at the end of 10 day period was 643 ug/ml. At these sites, total counts of spirochetes, motile rods and nonmotile rods were significantly reduced immediately following treatment. 59
- 60. • . Mombelli et al (2001) concluded that therapy of peri-implantitis by local delivery of tetracycline had a positive effect on clinical and microbiological parameters Rushin K et al (2016) discussed the management of an intra-bony defect with locally delivered teracycline fibres and splinting on a root canal treated tooth. The outcome of this case highlights a cost effective regenerative technique, without using bone grafts and GTR membranes, and also the importance of stabilization of a tooth during its healing phase post surgically for increasing its prognosis. 60
- 61. Can be concluded that local delivery of tetracycline improves the clinical outcomes of traditional treatment and should be considered particularly as an adjunct to scaling root planing. Considerations regarding the adverse effects of widespread use of tetracycline should be taken into account when choosing a therapeutic strategy of chronic periodontitis Pavia et al (2003) 61
- 62. DOXYCYCLINE POLYMER (ATRIDOX) • A biodegradable formulation containing •10% by weight doxycycline, •33% by weight poly (DL-Lactide) and •57% by weight N-methyl 2-pyrrolidone • Mechanism of action: Activity against putative periodontal pathogens and effective in the management of human diseases (Golub et al 1984, McCulloch et al 1990) • It is a liquid biodegradable system that hardens when placed in periodontal pocket 62
- 63. TECHNIQUE • Liquid delivery system containing 10% doxycycline hyclate is contained within a syringe that has a blunt ended 23 gauge cannula attached. The cannula has a diameter of a periodontal probe • The tip of the cannula is introduced to the depth of the pocket and the drug is expressed out 63
- 64. • As it begins to harden on contact with the moisture and during the 1-2 minutes of hardening, it is packed into the pocket using the underside of the moistened curette or other blunt-ended instrument • Immediately after administration, the polymer slightly protrudes from the pocket orifice • Periodontal dressing or adhesive is used as an aid in retention of the system • Instructions given to the patient is in lieu with tetracycline fibres 64
- 65. 65
- 66. MINOCYCLINE • Minocycline HCl, a semi synthetic tetracycline is one of the most active antibiotics for microorganisms associated with periodontitis. Its chemical formula is C23H27N3O7 • Minocycline has significant antimicrobial activity against a wide range of organisms as well as an anticollagenase effect. Dollery, C. Therapeutic Drugs. Churchill Livingstone, USA, 1999, Vol. 2, pp. M187-M188 Maehara R, Hinode D, Terai H, Sato M, Nakamura R, Matsuda N, et al. Inhibition of bacterial and mammalian collagenolytic activities by tetracyclines. Nippon Shishubyo Gakkai Kaishi 1998;30:182-90 66
- 67. RATIONALE BEHIND THE USE OF MINOCYCLINE IN PERIODONTAL DISEASES Sweetman, S.C. Martindale: the complete drug reference. 33rd ed., Pharmaceutical Press, London, 2009. [Academy report: The role of controlled drug delivery for periodontitis. J. Periodontol., 2000, 71, 125-140.]. 1. Broad spectrum of activity: bacteriostatic at low concentrations and bactericidal at high concentrations. 2.Property of substantivity i.e. ability to bind to the soft and hard tissue walls of the pocket thereby establishing a drug reservoir. 67
- 68. [Geng, S.; Cao, C.; Chen, Z. The effect of non-surgical periodontal and adjunctive minocycline-HCL treatments on collagenase activity. Zhonghua Kou Qiang Yi Xue Za Zhi., 2000, 35, 336-339.]. [Dollery, C. Therapeutic Drugs. Churchill Livingstone, USA, 1999, Vol. 2, pp. M187-M188 [Babich, H.; Tipton, D.A. In vitro response of human gingival epithelioid S-G cells to minocycline. Toxicol. In Vitro, 2002, 16, 1121.]. 3. Anti-collagenase activity against P.gingivalis, human gingival fibroblasts associated with induction of inflammation. 4. Higher lipid solubility ensures rapid passage through the lipid bilayer of the bacterial cell wall and inhibits protein synthesis. 5. Ability to enhance the activity of gingival epithelial cells to participate in the early inflammatory phase of periodontal wound healing. 68
- 69. 6. Lastly it is seen that uptake of minocycline via different transport systems in human gingival fibroblasts helps attaining higher levels in gingival cervicular fluid than blood, thus enhancing the effectiveness of the minocycline against invasive pathogens involved in periodontal diseases. Yang, Q.; Nakkula, R.J.; Walters, J.D. Accumulation of ciprofloxacin and minocycline by cultured human gingival fibroblasts. J. Dent. Res., 2002, 81, 836-840 .Brayton, J.J.; Yang, Q.; Nakkula, R.J.; Walters, J.D. An in vitro model of ciprofloxacin and minocycline transport by oral epithilial cells. J. Periodontol., 2002, 73, 1267-1272.) 69
- 70. MINOCYCLINE (DENTOMYCINE AND PERIOCLINE) • 3 modes of local application are available: •Film •Microspheres •Ointment It is a bacteriostatic 70
- 71. Film • Ethylcellulose containing 30% of minocycline cast from ethanol, chloroform or chloroform with polyethylene glycol were tested as sustained release devices (Elkayam et al) • The results of this study indicated that the use of this device may cause complete eradication of pathogenic flora from the pocket 71
- 72. Microspheres: • Minocycline micro-encapsulated in a resorbable poly glycolide-lactide slow release polymer can be administered by means of disposable plastic syringe. The volume of microspheres in each syringe is 4 mg which is equivalent to 1 mg of minocycline base (Braswell et al) 72
- 73. Microspheres : Injected into the pocket Adhered to the soft tissue Dissolves Releases minocycline in sustained manner 73
- 74. • Once in the pocket the micospheres react with the crevicular fluid which hydrolyzes the polymer causing water-filled channels to form inside the microspheres • These holes become the pathway for the antibiotic for sustained release • The minocycline then diffuses through these portals and permeates the surrounding tissues • Over a period of time, the microspheres themselves get fragmented through polymer hydrolysis and degrade and are ultimately bioresorbed. • It is reported that the microspheres are completely biodegraded in about 21 days 74
- 75. Ointment: •It is a light yellow colour ointment base of 20 mg hydroxyethyl cellulose, 10 mg eudragit RS, 60 mg triacetine and glycerine 0.5 g supplied in a disposable polypropylene applicator and each applicator contains the equivalent of 10 mg minocycline in 0.5 g ointment Repeated applications of 2% minocycline, 1 application per week for 4 weeks, 2 applications at intervals of 1 or 2 weeks, 3 applications at 2 weekly intervals were effective 75
- 76. 76
- 77. REVIEW OF LITERATURE Nakagawa T et al (1991) revealed that Periocline effectively eliminated periodontopathic gram- negative bacteria. These results indicated that a combination of Scaling and Root Planing with local administration of 2% minocycline for recurrent periodontal pockets brought about more satisfactory results than conventional SRP. Van Steenberghe D et al (1999) compared SRP and subgingival minocycline ointment for 15 months and found subgingival administration of minocycline ointment in the treatment of adult periodontitis is safe and leads to significant adjunctive improvement after subgingival instrumentation in both clinical and microbiologic variables over a 15-month period 77
- 78. • Hellström M.K et al (2008) conducted a study to evaluate the effects of minocycline microspheres on periodontal probing depth reduction when used in combination with surgery in adults with moderate to severe, chronic periodontitis. applications of local minocycline as an adjunct to surgery in adults with moderate to severe, chronic periodontitis were associated with statistically significant greater reductions in probing depth than surgery alone. 78
- 79. • Ruan H et al (2016) formulated a thermoresponsive gel for minocycline (MCL) with chitosan/β-glycerophosphate. The final preparations contained 0.5% (w/v) chitosan, 1.8% (w/v) β-GP and 2% (w/v) MCL. The constituents of the in situ gels formulation had a well-sustained release efficacy on the animal model of periodontitis 79
- 80. • Thus, minocycline can be used as a adjunct to mechanical debridement with improved effectiveness for treatment of chronic periodontitis Vanderkerckhove et al 80
- 81. METRONIDAZOLE • A 5-nitroimidazole compound specifically targets anaerobic microbes but has essentially no activity against aerobic or microaerophilic bacteria but its hydroxyl metabolite enhances its effect even against other group of bacteria (Pavicic et al) • Upon entry into an organism, metronidazole is reduced at 5-nitro position by electron transport proteins. The reduction of parent molecule produces free radicals. These react with bacterial DNA causing cell death. Hence it is primarily a bactericidal agent (Drisko et al). • Serum concentration of Metronidazole has shown to attain MIC levels for most periodontal pathogens and it is found to eliminate spirochetes from ANUG lesions. (Brit and Prohlod 1986) 81
- 82. METRONIDAZOLE DENTAL GEL (ELYZOL) • Resorbable • Consists of 25% of Metronidazole benzoate in a matrix consisting of Glyceryl mono-oleate Sesame oil • The gel is subgingivally placed with a syringe and a blunt cannula. The drug concentration in crevicular fluid follows an exponential pattern which is compatible with sustained drug delivery 82
- 83. 83
- 84. 84
- 85. REVIEW OF LITERATURE Ainamo et al (1992) compared the effect of metronidazole 25% gel with subgingival scaling in adult Periodontitis and found that both periodontal pocket depth and bleeding on probing were significantly reduced in both groups. Stelzel M et al (1997) compared topical application of a metronidazole 25% dental gel with subgingival scaling and found better results as compared to SRP alone . 85
- 86. Al Mubaraaak et al (2000) assessed the effect of topical application of a metronidazole gel (ELYZOL DENTAL GEL), and adjunctive therapy in the treatment of adult periodontitis clinically and found that topical Elyzol treatment may improve periodontal health as well as subgingival scaling and root planning therapy and adjunctive treatment could obtain an additional therapeutic effect. Paul Singh H et al (2016) studied the comparative effect of both aloe vera gel and metronidazole gel and the results of both test groups A.vera and metronidazole are comparable.Hence, local application of Aloe vera can be an effective and affordable herbal substitute for metronidazole 86
- 87. • Thus the effectiveness of metronidazole as an adjunct to SRP in the treatment of chronic adult periodontitis, but clinical significance and dissemination of antibiotics should be taken into account in the evaluation of metronidazole as an alternative to SRP (Pavia et al 2004) 87
- 88. CHLORHEXIDINE • It is a topical antiseptic belonging to the family of bisguanides. It is mainly active against gram positive group of organisms • It is bacteriostatic at lower and bactericidal at higher concentrations • It has been detected in excess of 125 µg/ml in crevicular fluid for 1 week following a single application (Soskolne et al 1998) 88
- 89. CHLORHEXIDINE CHIP (PERIOCHIP) • It is a bio-absorbable device • Comprises of 34% Chlorhexidine in a cross-linked gelatin matrix • Chip is 5 mm long, 4 mm wide with 2.5 mg of chlorhexidine gluconate 89
- 90. TECHNIQUE • After scaling and root planing, the chip is grasped in a cotton forceps and gently inserted into the pocket • It is advisable to dry the area before placing the chip • As burning sensation is reported after the chip placement, placement of multiple chips around a single tooth may result in discomfort • The chip degrades in a period of 7-10 days and requires no retentive system • Instructions given to the patient is in lieu with tetracycline fibres 90
- 91. 91
- 92. PERIOCOL- CG • (PerioCol™-CG) is a controlled-release chlorhexidine chip. Each PerioColTM-CG contains approximately 2.5 mg of chlorhexidine gluconate in a bio-degradeable matrix of Type 1 collagen derived from fish sources. • It releases chlorhexidine in vitro with a release profile of approximately 40-45% within 24hrs and afterward in linear fashion for 7-8 days. The release profile may be explained by initial burst effect due to diffusion of the drug from the chip followed by release of the drug due to enzymatic degradation 92
- 93. CHLOSITE • Chlosite consists of 1.5% chlorhexidine bonded in a xanthan carrier substance. It contains chlorhexidine in two different forms. The first form is 0.5 % highly soluble chlorhexidine digluconate, also called chlorhexidine-bis (D-gluconate). • This form of chlorhexidine is used as an antiseptic agent. The second form is a slow-release 1 % chlorhexidine dihydrochloride (a bis-biguanide with bacteriostatic characteristics). • Chlosite uses xanthan gel as the carrier • Xanthan in Chlosite provides good sub-gingival bonding of the local delivery device via mucoadhesion, while the high Chlorhexidine content guarantees a safe bactericidal effect. 93
- 94. 94
- 95. REVIEW OF LITERATURE D. Steinberg et al (1990): Release of Chlorhexidine from a degradable delivery system and the degradation of the matrix is controlled by variation in the formulation. This presented a new dental drug delivery system for sustained release of chlorhexidine that can be used as an adjunct in the treatment of periodontal diseases. Jeffcoat M et al (1998) proved the efficacy of a controlled-release biodegradable Chlorhexidine (CHX) (2.5 mg) chip when used as an adjunct to scaling and root planing significantly reduced probing depth (PD) and improved clinical attachment level (CAL) in adult periodontitis. 95
- 96. Paolantonio M et al (2008) provided further data supporting clinical and microbiologic effects of Chlorhexidine chips when used as an adjunct to Scaling and root planing. They obtained significant reduction in Probing Depth (PD) and a clinical attachment level (CAL) gain compared to SRP alone Jose K et al (2016) evaluated the outcome of chlorhexidine chip and diode laser as adjuncts to scaling and root planing and concluded Chlorhexidine local delivery alone or in combination with diode laser decontamination is effective in reducing PD and gaining CAL 96
- 97. Kaplish V, Walia M, Hari Kumar SL. Local drug delivery systems in the treatment of periodontitis: A review. Pharmacophore 2013;4(2):39-49. 97
- 98. 98
- 99. 99
- 100. COMPARISON OF DRUGS USED FOR LOCAL DELIVERY 100
- 101. OTHER DRUGS 101
- 102. OFLOXACIN • Ofloxacin belongs to quinolone family which constitute a group of 1,8 naphthyridine derivatives and are synthetically produced drugs • They are considered to be bactericidal as they inhibit the enzyme DNA replication by acting on the enzyme DNA gyrase. The bactericidal effect can only occur in the presence of competent RNA and protein synthesis. The imbalance of inhibited DNA replication and continued protein synthesis results in inhibition of cell division 102
- 103. OFLOXACIN INSERTS (PT-01) • PT-01 is a soluble insert, with both fast and sustained release parts containing 10% ofloxacin and showed a constant drug level of above 2 mg/ml, (minimum MIC for most pathogenic organisms) which could be sustained for up to 7 days • The controlled release system exhibited a biphasic pattern with a rapid early release phase peaking at approximately 12µg/ml and stabilizing at approximately 2µg/ml from day 3 to 7 following insertion (Higashi et al 1990) • Initial investigations failed to any additional microbiological effect in a split mouth design (Kimura et al 1991) • Four weekly applications of the insert resulted in significant resolution of periodontal inflammation and improvement in other clinical parameters compared to controls. (Yamagami et al 1992) 103
- 104. ANTIBIOTIC RESISTANCE ASSOCIATED WITH LOCAL DRUG DELIVERY SYSTEMS • Local drug delivery provides a high drug concentration at a specific site • Sublethal amounts of administered drugs leak out of pockets during therapy. Therefore, the potential exists that local drug delivery may contribute to development of drug resistant organisms in areas other than the treated sites 104
- 105. • Exposure to sub inhibitory concentrations of metronidazole or minocycline resulted in development of resistance among P.gingivalis P.intermedia F.Nucleatum P.Anaerobius Walker et al, Larsen et al • This suggests that repeated use of these agents can result in increased levels of drug resistant bacteria 105
- 106. • Thus, it can be concluded local delivery systems are logical adjuncts for the treatment of a few, localized non-responding sites, and systemic delivery reserved to control infections at multiple sites in patients with persistent disease and for treating atypical and aggressive forms of periodontitis (Tonetti 2000) 106
- 107. LDD VS SRP 107
- 108. • Hanes et al. in their systematic review, stated that as compared to SRP alone, when SRP is combined with certain local drug delivery agents, statistically significant adjunctive effects on PD reduction or CAL gain and decreased BOP were observed. Hanes PJ, Purvis JP. Local anti-infective therapy: Pharmacological agents. A Systematic Review. Ann Periodontal 2003;8:79-98 108
- 109. Future Trends in Local Drug Delivery • The requirements for treating periodontal disease include a means for targeting an anti infective agent to infection sites and sustaining its localized concentration at effective levels for a sufficient time while concurrently evoking minimal or no side effects. (Venkatesh A, Ramamurthy J 2012) • Various newer agents are being investigated in the field of local drug delivery to ensure maximum benefit. Venkatesh, A. and Ramamurthy, J., 2012. Local drug delivery systems in the treatment of periodontitis–An Overview. Int J Pharm Pharm Sci, 4(1), pp.30-37. 109
- 110. Clarithromycin Gel • A study has been conducted to investigate the adjunctive effects of subgingivally delivered 0.5 % clarithromycin as an adjunct to scaling and root planing for treating chronic periodontitis smoker subjects. • It was observed that the adjunctive use of 0.5% clarithromycin as a controlled drug delivery system enhanced the clinical outcome. • At the end of 6 months, the mean GI, PI, SBI, PPD, CAL for the clarithromycin group was significantly reduced. This product is still under investigation and yet to be patented. (Agarwal E et al) Agarwal, E., Pradeep, A.R., Bajaj, P. and Naik, S.B., 2012. Efficacy of local drug delivery of 0.5% clarithromycin gel as an adjunct to non-surgical periodontal therapy in the treatment of current smokers with chronic periodontitis: a randomized controlled clinical trial. Journal of periodontology, 83(9), pp.1155-1163. 110
- 111. Azithromycin Gel • Pradeep AR (2013) evaluate the adjunctive effects of subgingivally delivered 0.5% azithromycin as an adjunct to scaling and root planing (SRP) in the treatment of chronic periodontitis in smokers. • Significant improvement in clinical outcome were observed at 9 months. Pradeep AR, Bajaj P, Agarwal E, Rao NS, Naik SB, Kalra N, Priyanka N. Local drug delivery of 0.5% azithromycin in the treatment of chronic periodontitis among smokers. Aust Dent J 2013;58:34-40. 111
- 112. STATINS • These agents are widely used to lower cholesterol. • They also seem to modulate bone formation by increasing the expression of BMP-2, inflammation and angiogenesis. • Pradeep AR, Thorat MS (2010) investigated effectiveness of simvastatin(SMV) 1.2 mg gel into the periodontal pocket using a syringe with blunt cannula. • Greater decrease in gingival index and PD and more CAL gain with significant intrabony defect fill was observed. Pradeep AR, Thorat MS. Clinical effect of subgingivally delivered simvastatin in the treatment of patients with chronic periodontitis: A randomized clinical trial. J Periodontol 2010;81:214-22. 112
- 113. • Fajardo ME et al 2010 in their study shown that Atorvastatin have beneficial effects on alveolar bone loss. • Goes et al 2010 have shown that ATV was able to prevent alveolar bone loss in rats. • Pradeep AR et al (2013) observed significant increase in PD, CAL gain and improved bone fill. Pradeep AR, Kumari M, Rao NS, Martande SS, Naik S. Clinical efficacy of subgingivally delivered 1.2% Atorvastatin in chronic periodontitis: A randomized controlled clinical trial. J Periodontol 2013;84:871-9. 113
- 114. ALENDRONATE • Increases alveolar bone density with systemic use and, has been found to increase bone formation on local delivery into the periodontal pocket. • The efficacy of 1% ALN gel used as an adjunct to SRP for the treatment of intrabony defects in patients with chronic periodontitis with type 2 diabetes. • Significant increase in the PD reduction, CAL gain, and improved bone fill observed Pradeep AR, Sharma A, Rao NS, Bajaj P, Naik SB, Kumari M.Local Drug Delivery of Alendronate Gel for the Treatment of Patients With Chronic Periodontitis With Diabetes Mellitus: A Double-Masked Controlled Clinical Trial. J Periodontol 2012;83:1322-1328. 114
- 115. METFORMIN • Shown recently to stimulate osteoblasts and reduce alveolar bone loss. • Efficacy of 0.5%, 1%, and 1.5% MF gel as a local drug delivery system in adjunct to scaling and root planing for treatment of intrabony defects. • Significant increase in the PD reduction, CAL gain, and improved IBD depth reduction Pradeep AR, Rao NS, Naik SB, Kumari M. Efficacy of Varying Concentrations of Subgingivally Delivered Metformin in the Treatment of Chronic Periodontitis: A Randomized Controlled Clinical Trial. J Periodontol 2013;84:212-220. 115
- 116. FIBROBLAST GROWTH FACTOR • Very efficacious introduction in local drug delivery. • To regenerate periodontal tissues, a sandwich membrane composed of a collagen sponge scaffold and gelatin microspheres containing basic fibroblast growth factor (bFGF) in a controlled-release system was developed. • This sandwich membrane induced successful regeneration of the periodontal tissues in a short period of time (4weeks ). (Nakahara T 2003) Nakahara T, Nakamura T, Kobayashi E, Inoue M, Shigeno K et.al. Novel Approach to Regeneration of Periodontal TissuesBased on in Situ.Tissue Engineering: Effects of Controlled Release of Basic Fibroblast Growth Factor from a Sandwich Membrane. Tissue Engineering 2003, 9(1): 153-162. 116
- 117. NANOPARTICLES • Owing to their small size, penetrate regions that may be inaccessible to other delivery systems. • These systems reduce the frequency of administration and further provide a uniform distribution of the active agent over an extended period of time. • Three preliminary studies have been conducted to assess the efficacy of nanoparticles in periodontal drug delivery. 117
- 118. Chitosan Tripolyphosphate (TPP) a) Dung et al used Antisense oligonucleotide- loaded (TPP) nanoparticles and showed the sustained release of oligonucleotides which is suitable for the local therapeutic application in periodontal diseases. (Pragati S 2009) b) Pinon et al conducted a preliminary in vivo study in dogs with induced periodontal defects using Triclosan-loaded polymeric (PLGA, PLA and cellulose acetate phthalate) nanoparticles and suggested that triclosan- loaded nanoparticles penetrate through the junctional epithelium. (Pragati S 2009) Pragati S, Ashok S, Kuldeep S. Recent advances in periodontal drug delivery systems. Int J Drug Del 2009; 1: 1-14 Dung, D.T.K., Hai, T.H., Long, B.D. and Truc, P.N., 2009. Preparation and characterization of magnetic nanoparticles with chitosan coating. In Journal of Physics: Conference Series (Vol. 187, No. 1, p. 012036). IOP Publishing. . 118
- 119. HERBAL PRODUCTS • Various herbal formulations like aloe vera, neem, tulsi, propolis, cocoa husk, pomegranate, cranberry , etc. are being used widely these days. (Kukreja BJ, Dodwad V 2012, Bansal S 2012) • These products have shown promising results with no side effects and are economical as well. Kukreja BJ, Dodwad V. Herbal Mouthwashes – A Gift Of Nature: Int J Pharm Bio Sci 2012; 3: 46-52. 119
- 120. • The antimicrobial effects of green tea catechins on periodontopathogens have been studied by Hirasawa et al (2002) • They showed bactericidal activity against black pigmented organism at a minimum inhibitory concentration (MIC) of 1 mg/ml • Kudva P et al (2011) also demonstrated clinical and microbiological improvements following the use of Green tea catechin chip as an adjunct to scaling and root planing Hirasawa, M., Takada, K., Makimura, M. and Otake, S., 2002. Improvement of periodontal status by green tea catechin using a local delivery system: a clinical pilot study. Journal of periodontal research, 37(6), pp.433-438. 120
- 121. • The clinician’s decision to use LDAs should be based upon a consideration of clinical findings, the patient’s dental and medical history, scientific evidence, patient preferences, and advantages and disadvantages of alternative therapies. 122
- 122. DISEASES THAT CAN BE TREATED WITH LOCAL DRUG DELIVERY SYSTEMS • All drugs were used to treat patients with chronic periodontitis • Only tetracycline fibres and metronidazole were used to treat aggressive periodontitis • Mandell 1986 - Tetracycline fibers were not efficient in suppressing Aa – in J P • Mombelli et al (1997) - Tetracycline fibers were able to suppress, but not eliminate Aa • Riep et al (1996) -Local delivery of metronidazole too is not effective at suppressing Aa levels 123
- 123. Thus, at present there is no concrete evidence to use local delivery agents in the treatment of aggressive periodontal diseases 124
- 124. REMEMBER…….. • There is no single universal drug that would be effective in all situations • Local drug delivery often appears to be as effective as scaling and root planing with regards to reducing signs of periodontal inflammatory diseases • Local delivery may be an adjunct to conventional therapy. The sites most likely to be responsive to this adjunctive treatment method may be refractory or recurrent periodontitis 125
- 125. REMEMBER…….. • At present, there are insufficient data to indicate that one local drug delivery service is clearly superior to all the other systems • There is a lack of data to support the impression that local drug delivery in conjunction with root planing reduces the need for periodontal surgery more than scaling and root planing alone. • Should not be substituted for oral hygiene procedures. • Cigarette smoking has a negative influence on outcome of local drug therapy (Kinane et al 1999) 126
- 126. FUTURE REQUIREMENTS • Various drug delivery and drug targeting systems are currently under development to obtain so that better and effective administration of desired and newer drug can be done through the best possible system Increased dissolution velocity Increased saturation solubility Improved bioadhesivity and Versatility in surface modification • Long term longitudinal studies to be done to know the durability of these drugs on long term basis 127
- 127. AAP consensus on LDD • Thorough SRP is highly effective in the treatment of chronic periodontitis and is the standard approach to non-surgical periodontal therapy. Clinicians may consider the use of LDDs in chronic periodontitis patients as an adjunct to SRP 128
- 128. REFERENCES • (Rabbani GM,Ash MM, Caffesse RG .The effectiveness of subgingival scaling and root plaing in calculus removal.J Periodontal 1981;Volume 52;Number 3.119-123) • Quirynen M, De Soete M, Dierickx K, van Steenberghe D: The intra-oral translocation of periodontopathogens jeopardises the outcome of periodontal therapy. A review of the literature. J Clin Periodontol 2001; 28: 499-507. • Harper DS, Robinson PJ. Correlation of histometric, microbial, and clinical indicators of periodontal disease status before and after root planning. J Clin Periodontol 1987; 14:190-196 • Goodson JM. Antimicrobial strategies for treatment of periodontal diseases. Periodontol 2000.1994;5:142-68 • Walker CB. The acquisition of antibiotic resistance in the periodontal flora. Periodontol 2000.1996;10:78-88. 129
- 129. • Goodson J.M.,Haffajee A.,S. S. Socransky:Periodontal therapy by local delivery of tetracycline J Clin Periodontol 1979; 6: 83-92 • Prajapati J, Patel H, Agrawal YK. Targeted drug delivery for central nervous system: a review. Int J PharmPharm Sci 2012; 4(3): 32-38 • Local drug delivery in periodontics: a strategic intervention. International journal of pharmacy and pharmaceutical sciences. Vol 4, issue 4, 2012 • Local drug delivery in periodontal diseases. ……A review. NUJHS vol. 6, no.1, march 2016. • Recent advances in periodontal drug delivery systems Pragati S, Ashok S., Kuldeep S. International Journal of Drug Delivery 1(2009) 1-14 • Deeksha Joshi, Tarun Garg, Amit K. Goyal & Goutam Rath (2016) Advanced drug delivery approaches against periodontitis, Drug Delivery, 23:2, 363-377 • Review: recent advances in periodontal formulations . mr. Prakash sapra, dr. Biraju D patel, dr. Dhaval V Patel, Dr. Chetan H Borkhataria. International Journal of Pharmaceutical Chemistry and Analysis Vol.1, No.1, October 2014 130
- 130. • Local drug delivery system – A comprehensive review. Shaikh Samar, Chaudhari Amit, Khadtare Yogesh Indian journal of applied research. Volume : 5 | Issue : 5 | May 2015 • Carranza 11th edition • Lindhe 5th edition • Perio 2000. Vol. 10, 1996, 139-159 131
- 131. 132
Editor's Notes
- MECHANICAL THERAPY HAS ALWAYS BEEN …..
- The existence of an intra-oral translocation of the perio-pathogens has been demonstrated. Complex root and root anatomy- inaccessibility for plaque removal
- In such conditions , adjunctive use of chemotherapeutic agent provides anadditionalbenefit
- The concept of targeted delivery was based on the theory that cellular specificity of an accompanying drug would improve the therapeutic index.
- WD Miller in 1880’s suggested the use of an antimicrobial mouthrinse to fight ‘ PYORRHEA ALVEOLARIS’ studied a degradable sustained release device composed of a cross-linked protein containing Chlorhexidine as the therapeutic agent.
- Controlled-delivery systems are designed to release a drug slowly for more prolonged drug availability and sustained drug action. - application of currently available drugs to the subgingival area
- .Elevated proportions of some subgingival microbial species have been associated with destructive periodontal disease activity Elimination or adequate suppression of putative periodontopathogenic microorganisms in the subgingival microbiota is essential for periodontal healing Some periodontal pathogens may recolonize tooth surfaces from reservoirs on the tongue, tonsils and buccal mucosa . Bacteria associated with the periodontal diseases are usually found in biofilms and not as single organisms found in the aqueous suspensions. Biofilms are defined as matrix enclosed bacterial population adherent to each other and to the surface or inter surfaces. These masses secrete an exopolysaccharide matrix for protection and considerably higher concentrations of drugs are needed to kill bacteria in biofilms than organisms in aqueous suspensions. For this a higher concentration can be achieved by local drug delivery system.
- . Studies suggest that the critical period of exposure of the pocket to an antibacterial agent is in the range of 7-10 days
- Dodwad v – magic bullet Rose LF, Mealey BL, Genco RJ, Cohen DW. Periodontics. China: Elsevier Mosby; 2004 12. Greenstein G. The Role of Local Drug Delivery in the Management of Periodontal Diseases: A Comprehensive Review. J Periodontol 1998; 69: 507-20
- Gagandeep (Divya P.V, K. Nandakumar. Local drug delivery-Periocol in periodontics. Trends Biomater. Artif. Organs. 2006: 19: 74080
- Gagandeep , 8. Dentino A. Overview of locally delivered controlled release antimicrobials: Adjuncts to periodontal therapy. Practical hygiene 1998;4:55-61
- (Divya P.V, K. Nandakumar. Local drug delivery-Periocol in periodontics. Trends Biomater. Artif. Organs. 2006: 19: 74080
- Rams TE, Slots J. Local delivery of antimicrobial agents in the periodontal pocket. Periodontol 2000, 1996; 10: 139159.
- Soskolne WA, Heasman PA, Stabholz A, et al. Sustained local delivery of Chlorhexidine in the treatment of Periodontitis: a multicenter study. J Periodontol 1997;68:32-38.
- Greenstein G, Tonetti M. Academy report: The role of controlled drug delivery for periodontitis (Position paper). J. Periodontol. 2000; 71: 125-140.
- V dodwad magic bullet
- Goodson 1989 Total pocket fluid volume thus may turn over about 40 times an hour in a moderate-sized periodontal pocket (0.5 чl volume), which is more frequent than the oral cavity salivary turnover rate of about 28 times an hour
- Iodine showed 5-minute bactericidal action against the test organisms at concentrations therapeutically attainable in subgingival sites (0.25-0.5% Environmental conditions in periodontal pockets may alter effective in vivo concentrations of anti-microbial agents. For example, chlorhexidine may be inactivated in periodontal pockets via binding to serum proteins , which are markedly elevated in gingival crevicular fluid
- In periodontal pocket biofilm environment causes slow growth of organism and it affect the effectiveness of antibiotics. GCF clearance is very high and drug concentration will be affected by this.
- Based on, an assumed pocket volume of 0.5ml and a gingival fluid flow rate of 20µl /hr, it was estimated that half time of a non binding drug placed into a pocket is about a minute.
- Tetracycline, Doxycycline and Minocycline are commonly used with similar spectrum of activity. Hence resistance to one indicates resistance to all the three
- Hanes PJ, Purvis JP. Local anti-infective therapy: Pharmacological agents. A Systematic Review. Ann Periodontal 2003;8:79-98
- Kudva P, Tabasum ST, Shekhawat NK. J Indian Soc Periodontol. 2011;15(1):39-45.
- Pragati S, Ashok S, Kuldeep S. Recent advances in periodontal drug delivery systems. Int J Drug Del 2009; 1: 1-14.