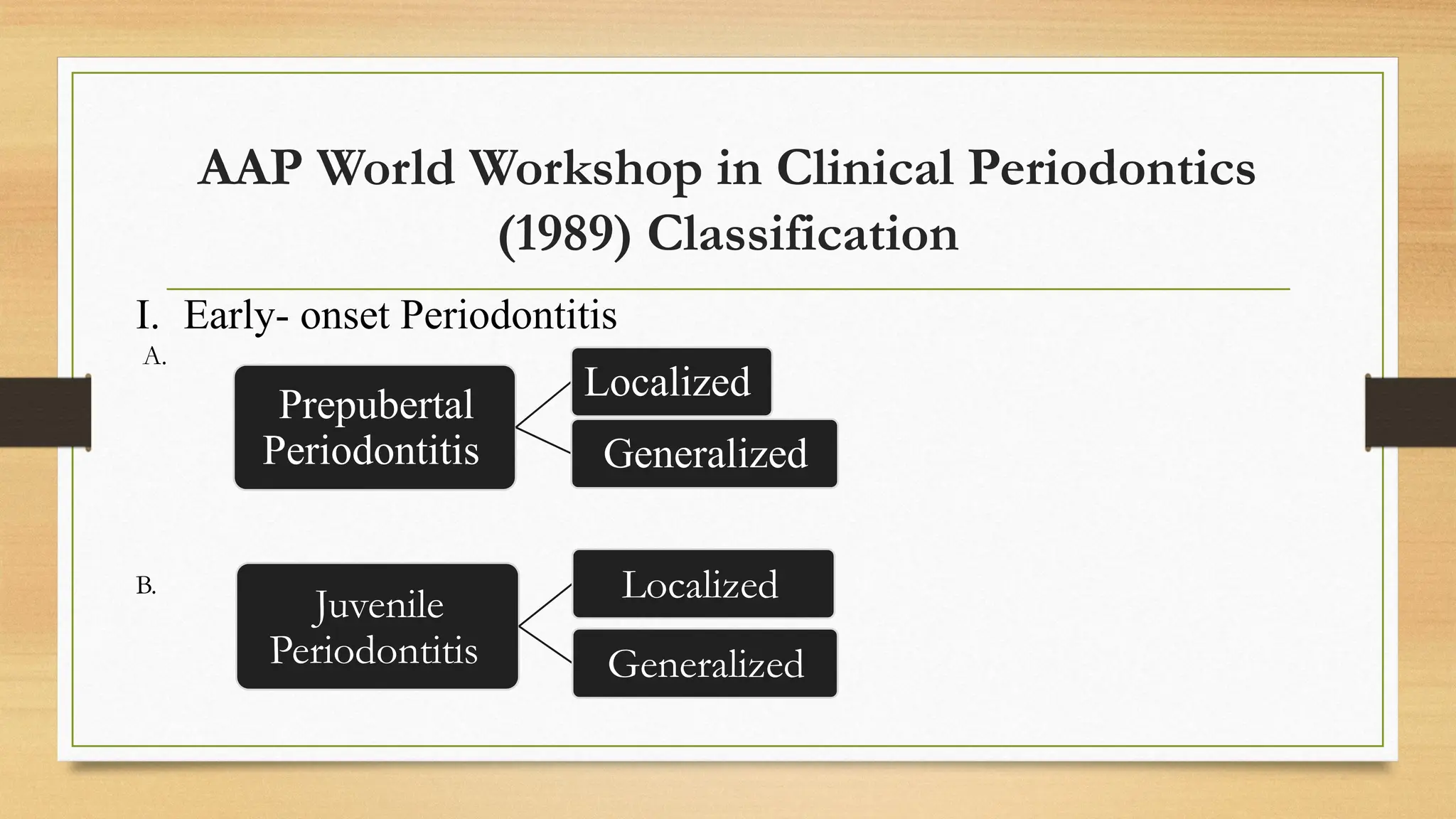
The document discusses the classification of periodontal diseases, detailing various classification systems and their evolution over time. It emphasizes the importance of having an organized classification for understanding the etiology, diagnosis, and treatment of periodontal conditions while highlighting the advantages and drawbacks of different classifications. The latest classifications aim to reflect advances in clinical understanding and address limitations of previous frameworks.


























































![References
• Lindhe, J. (2008, January 1). Clinical periodontology and implant dentistry. 1. [Basic
concepts]. 5th
Ed
• Newman, M. G., Takei, H., Klokkevold, P. R., & Carranza, F. A. (2011, February 14).
Carranza’s Clinical Periodontology. 10th
Ed
• Sutthiboonyapan, P., Wang, H., & Charatkulangkun, O. (2020, April 8). Flowcharts for
Easy Periodontal Diagnosis Based on the 2018 New Periodontal Classification. Clinical
Advances in Periodontics, 10(3), 155–160. https://doi.org/10.1002/cap.10095](https://image.slidesharecdn.com/seminarperiodontalclassification-240923122215-6fa3a48d/75/Periodontal-diseases-classification-pptx-70-2048.jpg)


