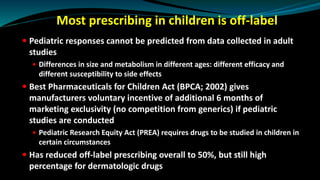
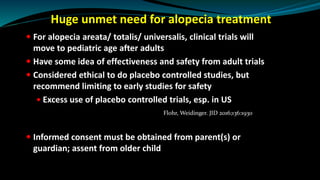
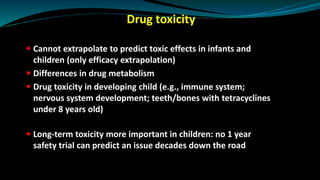
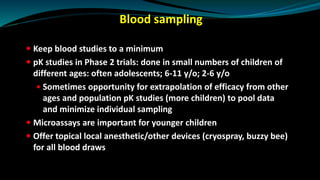
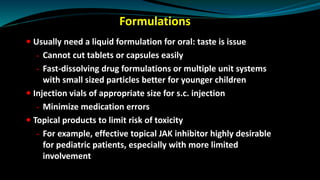
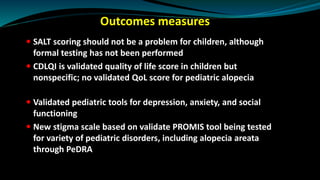
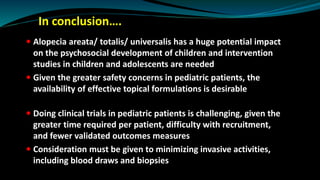
The document discusses the complexities and challenges of conducting pediatric clinical trials, particularly in dermatology, highlighting the differences in drug responses between children and adults. It outlines regulatory frameworks aimed at improving pediatric research and the ethical concerns surrounding off-label prescribing and informed consent. The necessity for effective treatments for conditions like alopecia areata in children is emphasized, along with the need for innovative formulations and research methodologies tailored to this demographic.