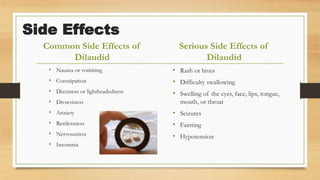
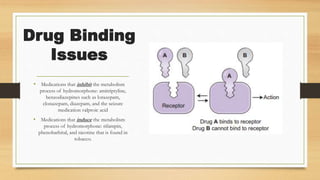
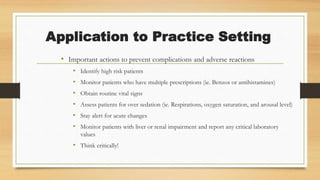
Hydromorphone is an opioid analgesic used to treat cancer pain. It works by binding to opioid receptors in the brain to increase pain tolerance. Common side effects include nausea, vomiting, dizziness, and constipation. It can interact with other CNS depressants and cause respiratory depression. Careful monitoring is needed when prescribing to patients with liver or kidney impairment or those taking interacting medications.