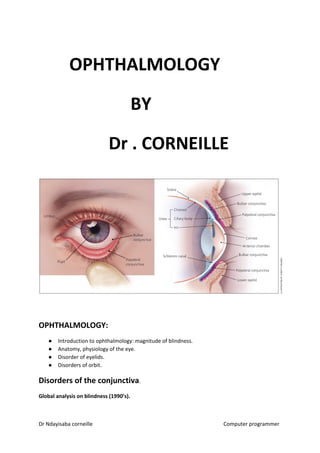
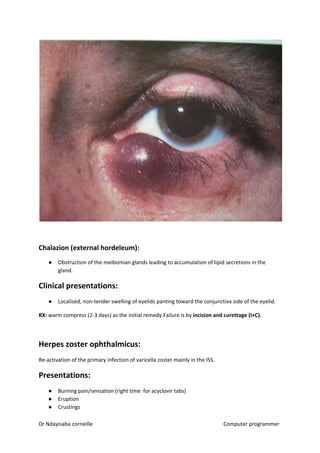
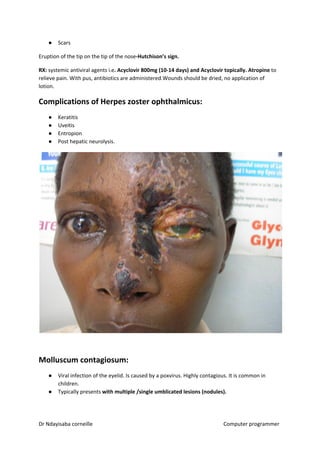
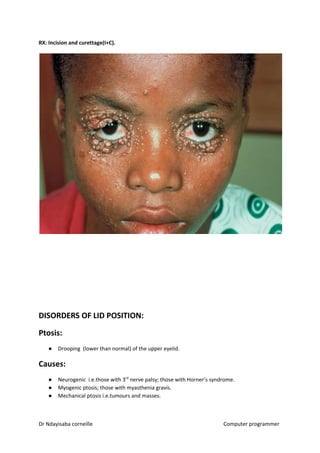
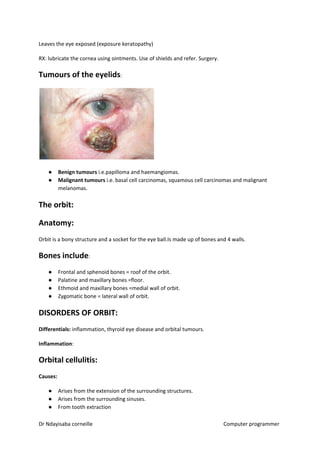
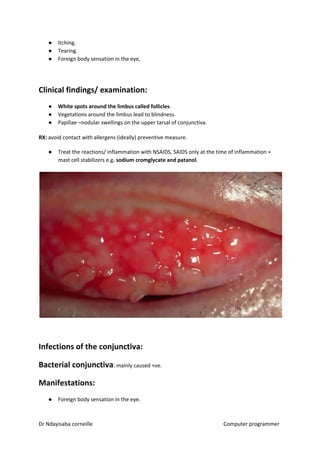
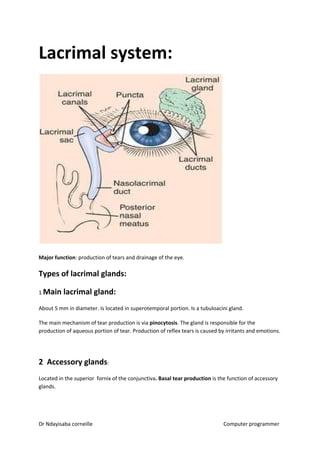
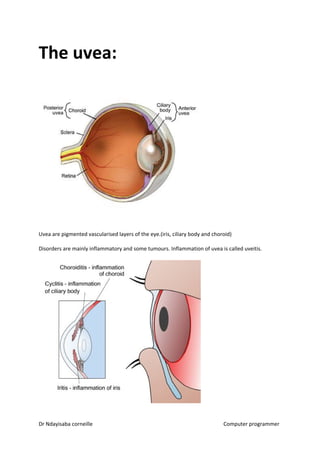
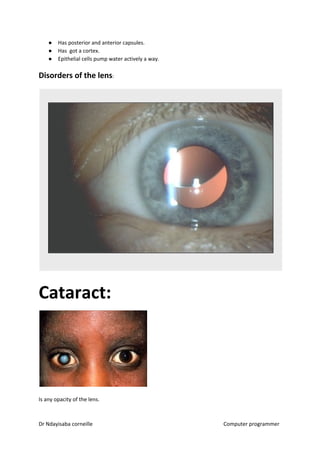
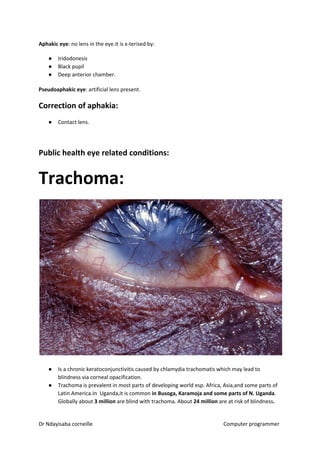
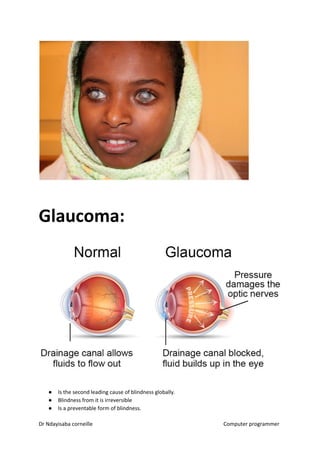
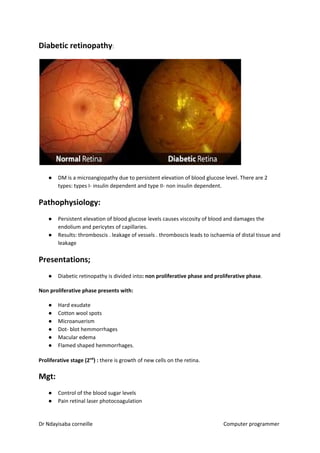
This document provides an overview of ophthalmology and eye anatomy and disorders. It discusses that globally, 37 billion people are blind with the main causes being cataract, glaucoma, trachoma, and diabetic retinopathy. It describes the anatomy of the eye including the cornea, iris, lens, retina and other structures. Common eye disorders covered include sty, chalazion, herpes zoster ophthalmicus, ptosis, entropion, ectropion, and tumors of the eyelids. Disorders of the orbit such as cellulitis, thyroid eye disease, and tumors are also summarized. The document concludes with diseases of the conjunctiva including allergic, vernal,