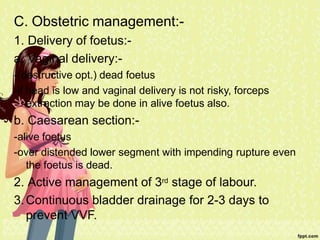
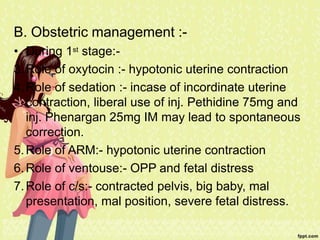
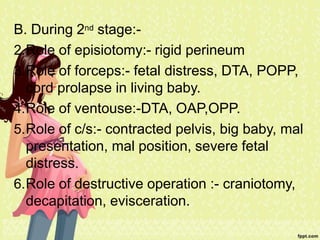
Obstructed labour occurs when there is poor progress of labour despite adequate uterine contractions, and is caused by issues with the birth canal (maternal factors) or baby (fetal factors). It can lead to maternal complications like rupture of the uterus, fistulas, and death if not managed properly. Management involves general supportive care, correcting dehydration, antibiotics to prevent infection, and obstetric interventions like assisted vaginal delivery or c-section depending on the situation. Prolonged labour is defined as labour lasting over 18 hours, and can be caused by problems with contractions, the cervix, or a constricted pelvis. It requires general supportive care and interventions may include oxytocics to strengthen contractions,