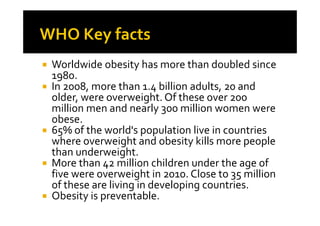
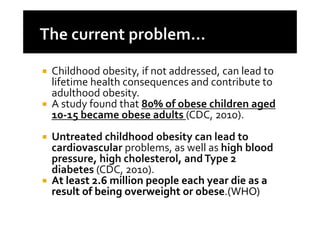
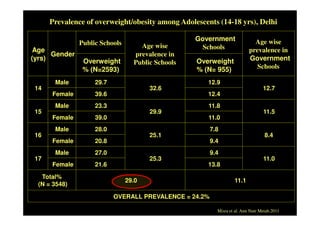
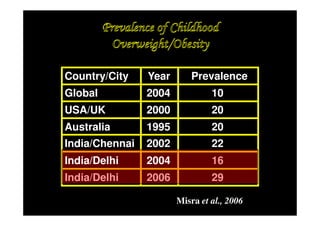
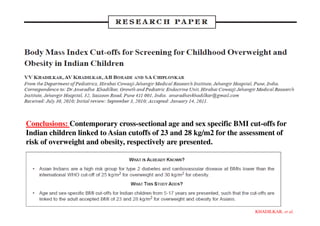
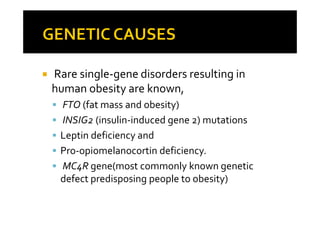
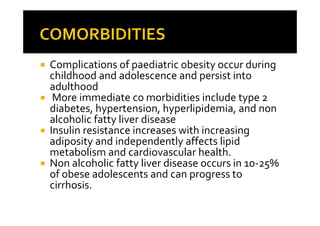
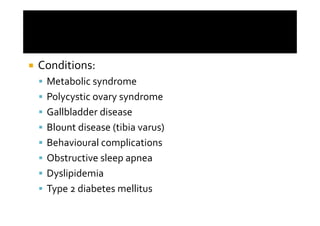
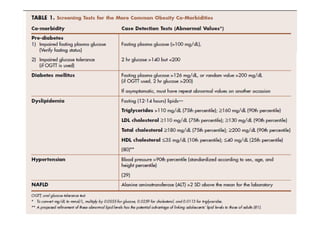
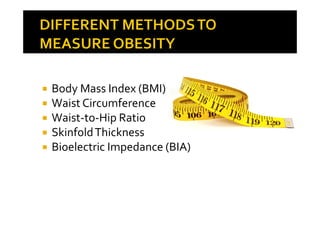
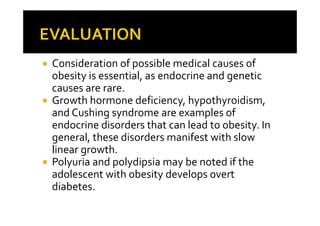
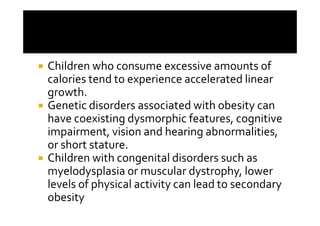
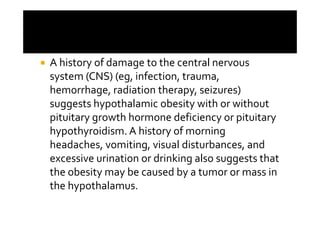
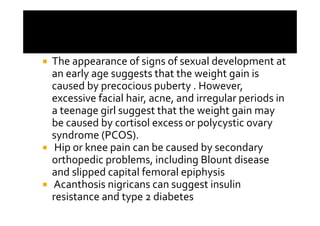
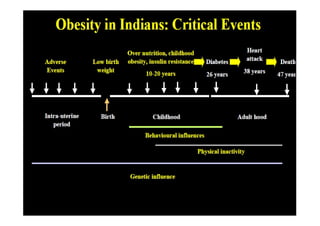
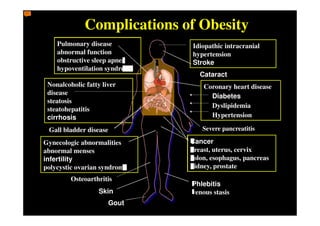
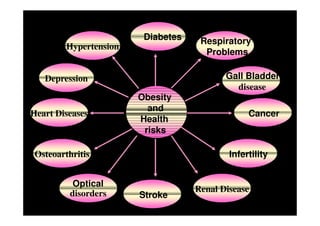
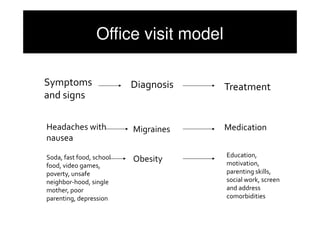
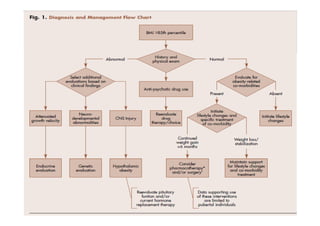
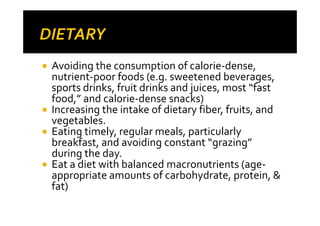
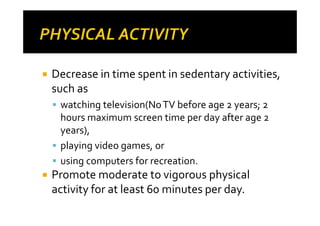
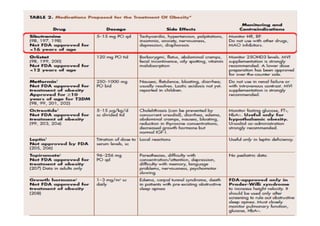
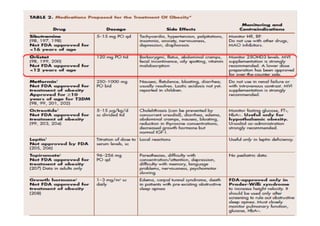
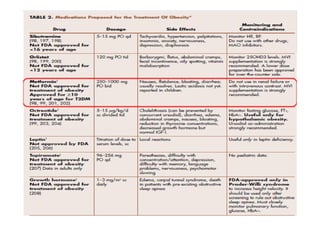
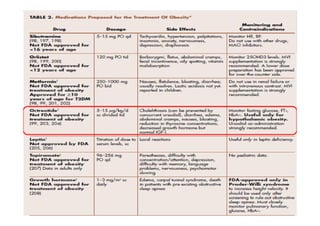
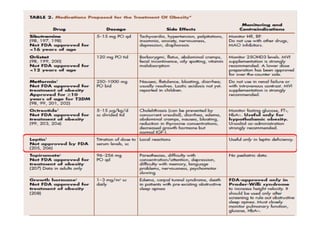
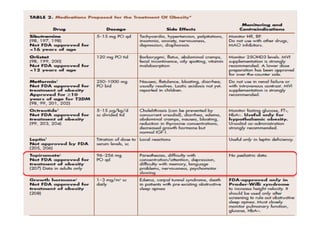
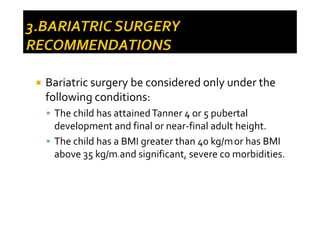
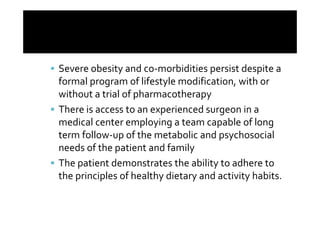
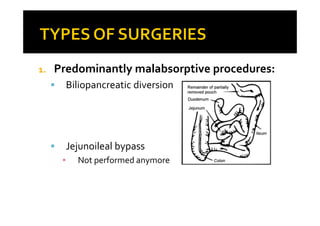
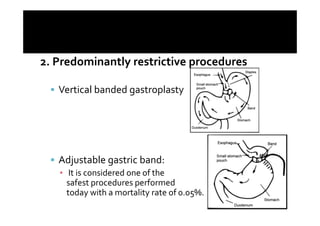
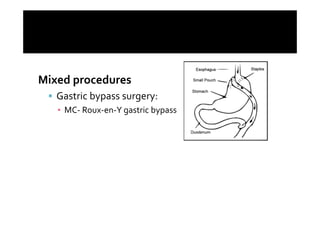
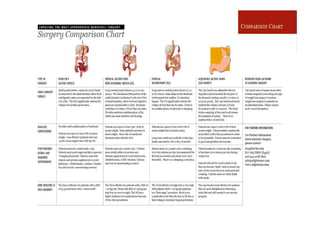
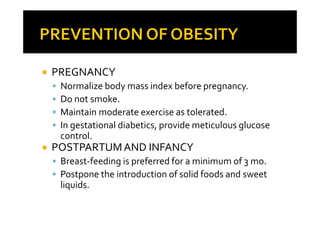
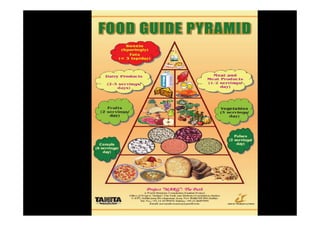
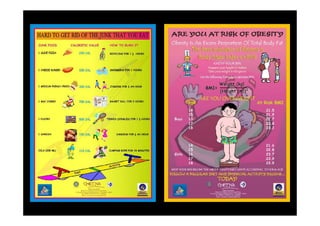
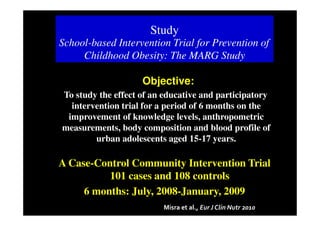
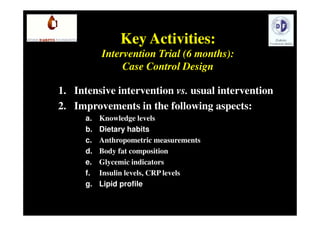
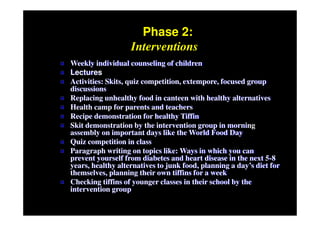
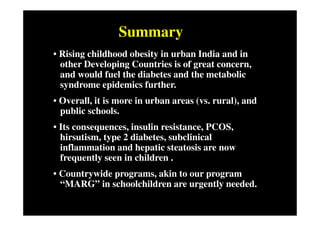
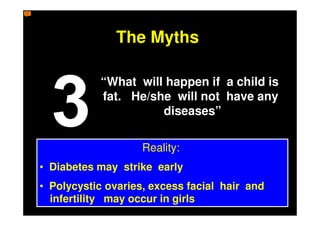
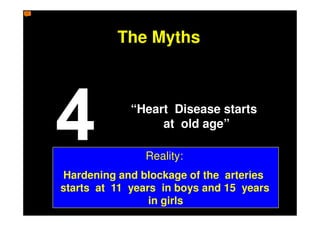
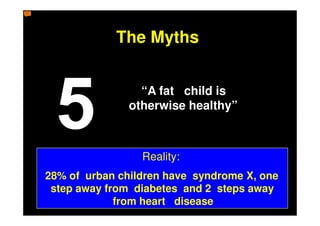
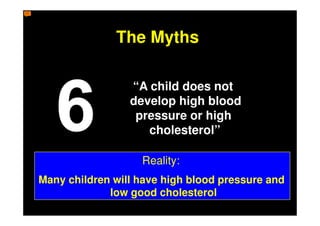
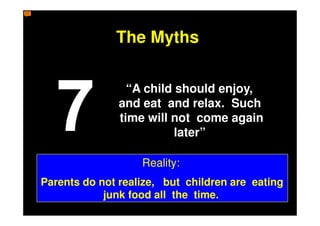
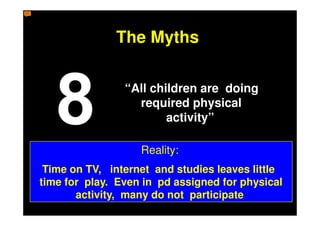
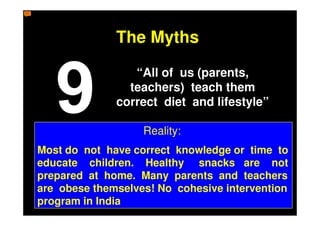
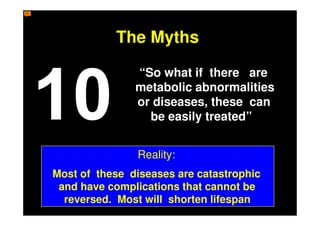
The document discusses the increasing prevalence of childhood obesity globally and outlines various lifestyle and medical interventions to address it. Recommendations include lifestyle modifications focusing on diet, physical activity, and behavior changes as first-line treatment, with consideration of pharmacotherapy or bariatric surgery for severe cases that do not respond to lifestyle changes alone. Childhood obesity is a serious public health issue that requires a multidisciplinary approach to treatment and management of co-morbidities.