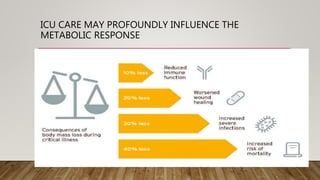
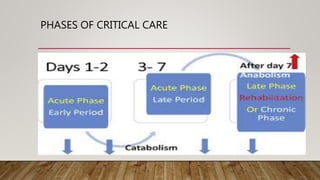
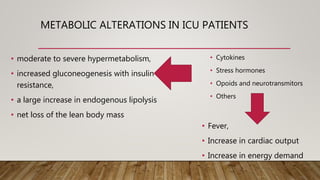
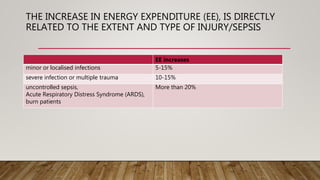
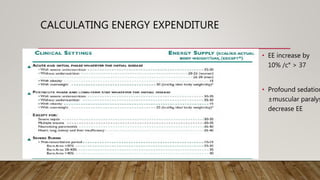
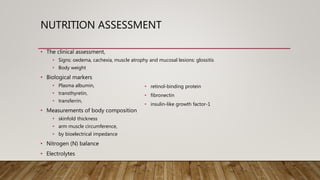
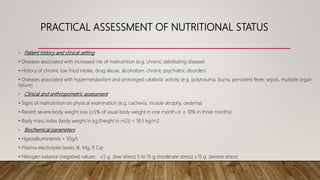
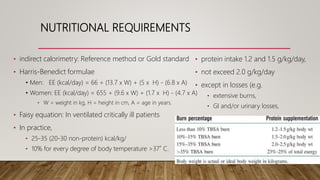
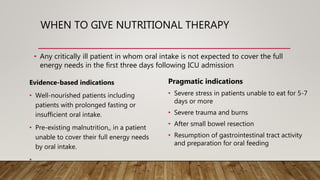
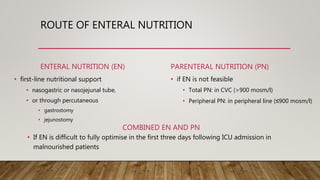
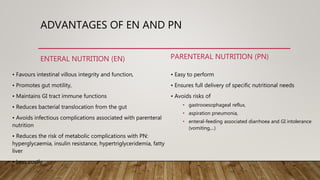
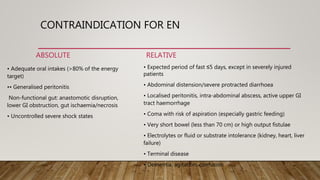
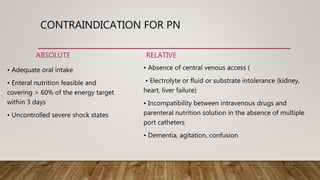
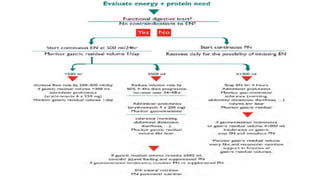
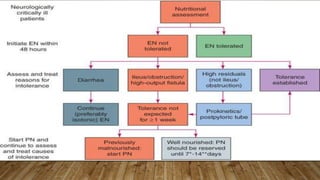
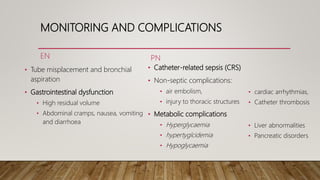
Nutritional therapy is important for critically ill patients in the ICU. Patients experience metabolic disturbances like hypermetabolism and loss of lean body mass. Nutritional requirements should be calculated using methods like indirect calorimetry or formulas, with a focus on adequate protein, calories, and adjustments for fever. Enteral nutrition is preferred over parenteral nutrition when possible due to benefits and lower risk of complications, though parenteral may be needed if enteral is not feasible or sufficient. Monitoring is important to watch for complications from each type of nutrition support.