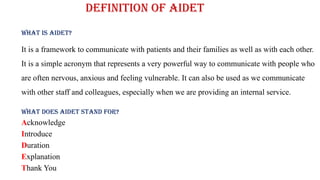
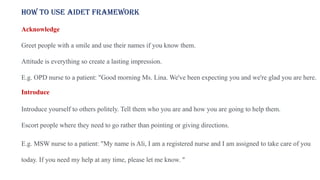
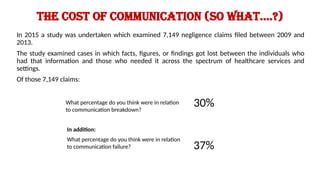
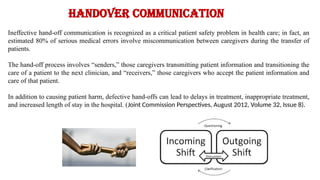
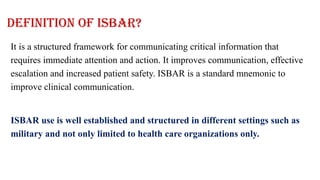
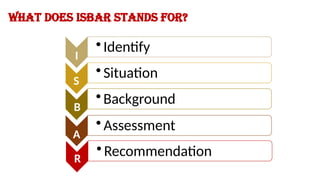
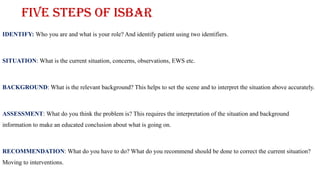
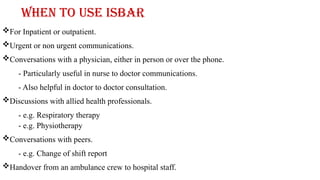
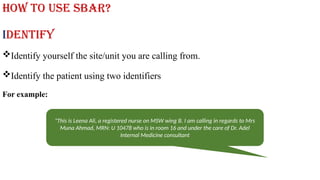
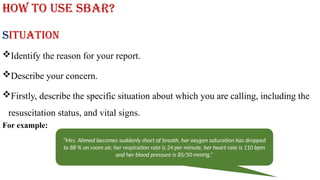
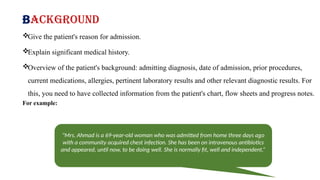
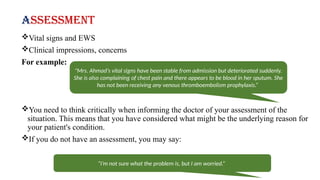
The document outlines training objectives for improving interpersonal communication skills in the workplace using the AIDET and ISBAR frameworks. AIDET stands for Acknowledge, Introduce, Duration, Explanation, and Thank You, and is meant to enhance communication with patients and colleagues, while ISBAR is a structured communication tool for critical information transfer. Effective communication through these frameworks is emphasized as essential for patient safety, satisfaction, and overall healthcare efficiency.