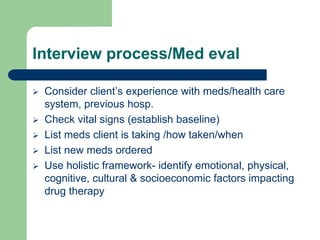
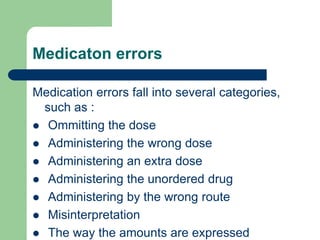
The document discusses the nursing process as it applies to drug administration. It outlines the key steps - assessment, planning, implementation, and evaluation. Assessment involves collecting subjective and objective data on the client, medication, and environment. Planning involves analyzing the data to develop nursing diagnoses and goals. Implementation means preparing and administering the medication correctly. Evaluation monitors the client's response to the drug. The document also reviews a nurse's responsibilities in areas like safe storage, accurate transcription of orders, informed consent, and documentation.