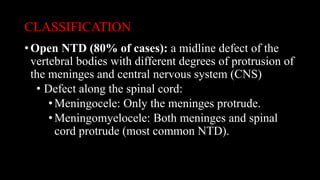
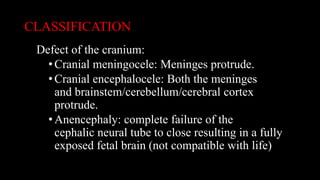
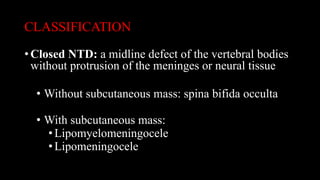
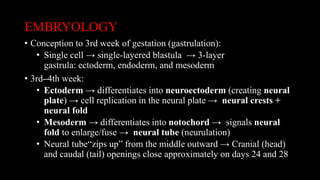
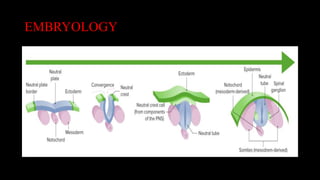
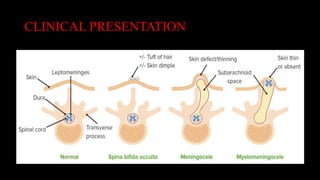
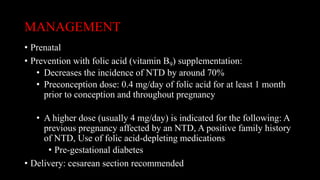
Neural tube defects are congenital conditions that occur when the neural tube fails to close fully during early embryonic development. They affect around 1 in 1,500 births in the United States. Neural tube defects can be open, with protrusion of nervous system tissue, or closed without protrusion. Prenatal screening and folic acid supplementation can help reduce neural tube defect risk and aid diagnosis. After birth, treatment depends on the specific defect but may involve surgery to close open defects.