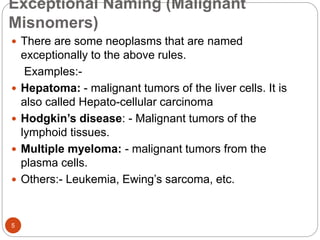
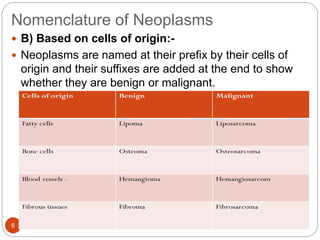
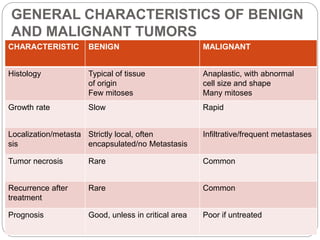
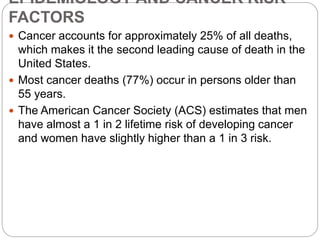
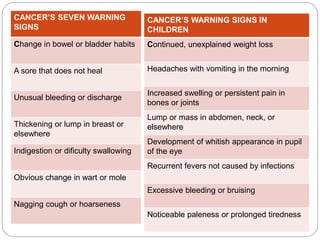
This document discusses neoplasia and cancer. It defines key terms like neoplasm, tumor, benign and malignant tumors. It explains that neoplasia is abnormal cell growth, and tumors can be benign (non-cancerous) or malignant (cancerous). Malignant tumors are able to invade other tissues and metastasize (spread) to other parts of the body. The document also discusses cancer risk factors, carcinogenesis (the process of cancer development), common carcinogens (cancer-causing agents) like chemicals, radiation and viruses, and the process of metastasis (cancer spreading).