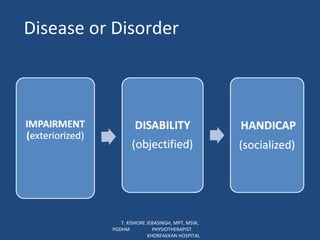
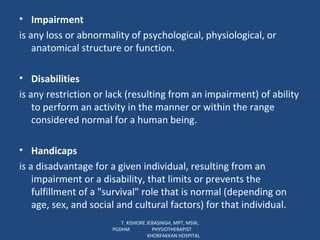
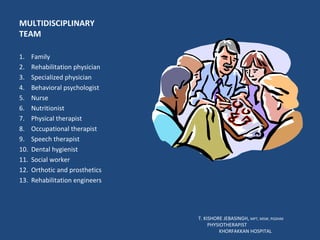
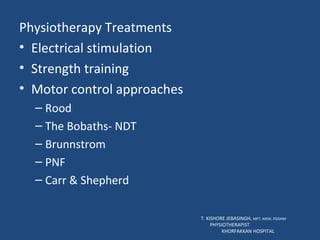
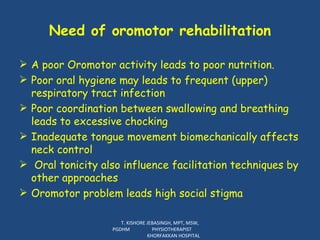
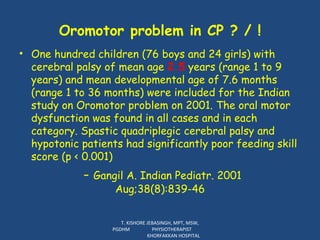
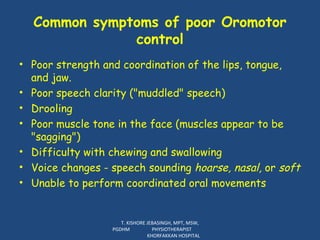
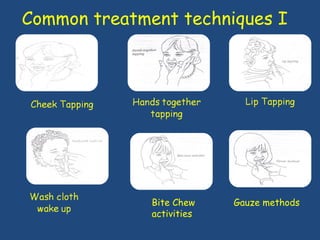
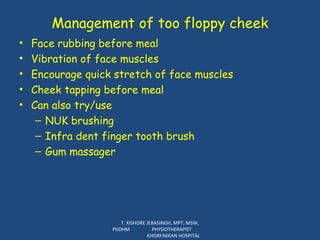
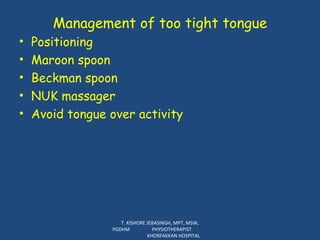
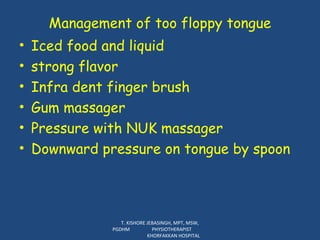
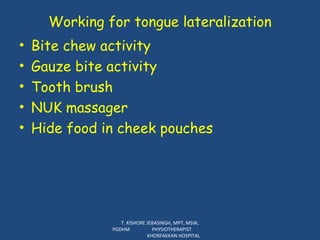
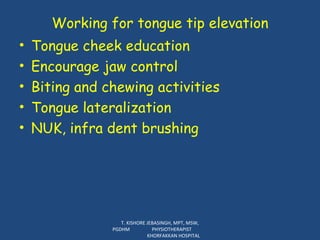
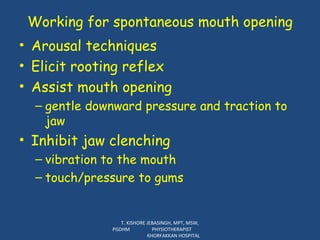
The document discusses disability rehabilitation and provides definitions of key terms from the World Health Organization. It describes the roles of an interdisciplinary rehabilitation team which includes various medical professionals. The team provides comprehensive client assessments and works together with a family-centered approach to set goals and facilitate positive outcomes for clients. Physiotherapy and occupational therapy services are outlined, along with techniques for oromotor rehabilitation to address common issues like drooling.