Mod 1 case 2022
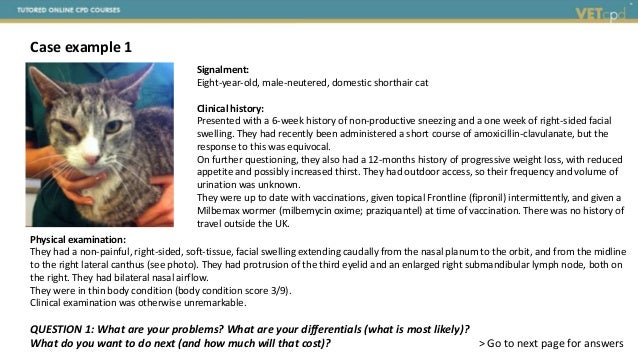
- 1. Signalment: Eight-year-old, male-neutered, domestic shorthair cat Clinical history: Presented with a 6-week history of non-productive sneezing and a one week of right-sided facial swelling. They had recently been administered a short course of amoxicillin-clavulanate, but the response to this was equivocal. On further questioning, they also had a 12-months history of progressive weight loss, with reduced appetite and possibly increased thirst. They had outdoor access, so their frequency and volume of urination was unknown. They were up to date with vaccinations, given topical Frontline (fipronil) intermittently, and given a Milbemax wormer (milbemycin oxime; praziquantel) at time of vaccination. There was no history of travel outside the UK. QUESTION 1: What are your problems? What are your differentials (what is most likely)? What do you want to do next (and how much will that cost)? > Go to next page for answers Case example 1 Physical examination: They had a non-painful, right-sided, soft-tissue, facial swelling extending caudally from the nasal planum to the orbit, and from the midline to the right lateral canthus (see photo). They had protrusion of the third eyelid and an enlarged right submandibular lymph node, both on the right. They had bilateral nasal airflow. They were in thin body condition (body condition score 3/9). Clinical examination was otherwise unremarkable.
- 2. QUESTION 1: What are your problems? ANSWER: • Major concerns o Six-week history of non-productive sneezing o One-week history of unilateral facial swelling o Enlarged sub-mandibular lymph node • Minor concerns o One-year history of reduced appetite ( weight loss / thin condition) / increased thirst that was progressive o Third-eyelid protrusion o Recently received antimicrobials – unknown response QUESTION 2: What are your differentials? > Go to next page for answers
- 3. QUESTION 2: What are your differentials? ANSWER: • Sneezing o Infection – viral (e.g. feline herpesvirus (FHV-1); fungal (e.g. Cryptococcus); bacterial o Foreign body o Dental disease o Environmental irritation • Unilateral facial swelling o Superficial disease Infection (abscess or cellulitis) – bacterial (e.g. cat fight injuries); fungal Inflammation – allergic (e.g. insect sting) Trauma Haematoma o Orbital disease Conjunctivitis o Extension of disease from the nasal cavity / sinus Infection – bacterial; fungal Neoplasia > Answer continued on next page Notes: Due to the shared timeframe – the sneezing and facial swelling are likely related. This makes invasive disease (neoplasia; deep infection) most likely
- 4. QUESTION 3: What do you want to do next? > Go to next page for answers … continued… QUESTION 2: What are your differentials? Whilst, we tend to focus on the major / acute problems, considering the minor issues can sometimes raise the suspicions of differentials for the major problem. It also highlights areas we might want to assess before proceeding to more invasive procedures. Reduced appetite o Oral / dental disease o Gastrointestinal disease o Systemic disease e.g. chronic kidney disease; apathetic hyperthyroidism; cholangitis; pancreatitis o Reduced sense of smell Increased thirst o Chronic kidney disease o Hyperthyroidism o Diabetes mellitus o Increased gastrointestinal losses o Electrolyte disturbances Third eyelid protrusion o Orbital disease o Neurological disease (e.g. middle ear disease) Enlarged lymph node o Inflammation – e.g. reactive (i.e. to inflammation of tissues that drain into it) o Neoplasia – primary (e.g. lymphoma); metastatic (i.e. from tissues that drain into it) Notes: Due to the shared timeframe – the reduced appetite and increased thirst are most likely related, and can be considered in combination (e.g. consider your differential list for polydipsia and prioritise those that also reduce appetite, whilst lowering, but not removing the differentials that often cause increased appetite). The weight loss and thin condition can also be considered a function of the reduced appetite. Unlikely that diabetes has been present for a year without having a crisis, but there could be compound issues happening. The enlarged lymph node is likely related to the facial swelling as on the same side – but that fits with both neoplasia and infection!
- 5. QUESTION 3: What do you want to do next? ANSWER Haematology – looking for evidence of inflammation or systemic disease Serum biochemistry – looking for evidence of inflammation or systemic disease; checking for chronic kidney disease, hyperthyroidism, diabetes mellitus, electrolyte disturbances etc. Urinalysis – looking for evidence of reduced urine concentrating ability (e.g. to support increased renal losses as a cause of the polydipsia), and to check for diabetes mellitus Clotting screen – check for coagulopathy (preferable, before inducing epistaxis! But, as no history of epistaxis / haemorrhage, could be optional if finances are limited) Respiratory virus screen (FHV-1 PCR and feline calicivirus (FCV) RT-PCR) Cryptococcus antigen serology (optional, could pend other diagnostics e.g. histology or cytology) Retrovirus screen (optional, but sensible in a sick, older cat) Fine needle aspirate cytology o Lymph node o Facial swelling Diagnostic imaging – CT head Endoscopy – rhinoscopy with biopsy Estimate to get an answer (i.e. does not include treatment) £3500 > Go to next page for test results
- 6. Investigation Blood analysis Parameter Unit Reference interval Hb 8.99 g/dl 8.00 – 15.00 HCT 28.8 % 25.0 – 45.0 RBC 6.94 x1012/l 5.50 – 10.00 MCV 41.4 fl 40.0 – 55.0 MCH 13.0 pg 12.5 – 17.0 MCHC 31.3 g/dl 30.0 – 35.0 Plt 393 x109/l 200 – 700 WBC 25.7 x109/l 4.90 – 19.00 Neutrophils 23.64 x109/l 2.40 – 12.50 Lymphocytes 1.80 x109/l 1.40 – 6.00 Monocytes 0.00 x109/l <0.70 Eosinophils 0.26 x109/l <1.60 Basophils 0.00 x109/l <0.10 Blood film examination Unremarkable Haematology Clotting seen Was unremarkable Parameter Unit Reference interval Urea 10.3 mmol/l 6.5 – 10.5 Creatinine 211 µmol/l 133 – 175 Total protein 91.7 g/l 77.0 – 91.0 Albumin 23.5 g/l 24.0 – 35.0 Globulin 68.2 g/l 21.0 – 51.0 Albumin/Globulin ratio 0.35 0.4 – 1.30 ALT 21 IU/l 15 – 45 ALKP 5 IU/l 15 – 60 Total bilirubin 3.4 µmol/l <10 Sodium 151.9 mmol/l 149.0 – 157.0 Potassium 3.86 mmol/l 4.00 – 5.00 Chloride 122 mmol/l 115 – 130 Calcium 2.38 mmol/l 2.30 – 2.50 Phosphate 0.70 mmol/l 0.95 – 1.55 Glucose 6.3 mmol/l 4.0 – 6.5 Cholesterol 4.8 mmol/l 3.5 – 7.0 Triglycerides 0.42 mmol/l <1 Thyroxine 25.9 nmol/L 15-60 Serum biochemistry > Test results continued on next page
- 7. Investigation (continued) Urinalysis (collected by cystocentesis) pH 6.7 Protein creatinine ratio 0.21 Specific gravity 1.022 Dipstick Blood ++ Glucose negative Ketones negative Sediment examination Unremarkable Culture Negative Infectious disease screening Respiratory virus screen – negative for FHV- 1 and FCV by PCR / RT-PCR Cryptococcus antigen serology – negative Retrovirus screen – FIV antibody negative; FeLV antigen negative Fine needle aspirate cytology Sub-mandibular lymph node were possible conscious: Description: Mixed population of predominantly small lymphocytes, with scattering of plasma cells and neutrophils. No organisms seen. Comment: Consistent with immune stimulation Facial swelling not attempted whilst conscious QUESTION 4: What do you think is going on? What do you want to do next (i.e. have these results changed your investigation plan)? > Go to next page for answers
- 8. QUESTION 4: What do you think is going on? What do you want to do next (i.e. have these results changed your investigation plan)? ANSWER: Preliminary Conclusions & treatment Conclusions There is evidence of kidney disease, most likely chronic given the history. Due to the reduced body condition the creatinine value likely underestimated the degree of compromise. Concurrent diabetes mellitus and hyperthyroidism have been ruled out. Kidney disease combined with fasting prior to blood sampling likely account for the slightly low potassium. The hyperglobulinaemia likely reflects a chronic inflammatory process, supported by the mature neutrophilia; however, a neoplastic process could not be ruled out. The lymph node cytology makes inflammation more likely and neoplasia less likely – but does not rule it out. Common infectious causes of rhinitis (i.e. FHV-1; FCV) have been ruled out, as have common reasons for immune-suppression. Initial treatment The presence of kidney disease does not account for the facial swelling; however, it does impact on investigation and future treatment. Further evaluation of the kidneys would now be indicated: measurement of blood pressure; abdominal ultrasonography. Iodinated CT contrast agents have the potential to exacerbate kidney disease and cause acute kidney injury; they are used only with caution in animals with known kidney compromise. In this case, potassium-supplemented fluid therapy was administered prior to the anaesthetic to address any subclinical dehydration, a lower dose of contrast agent was used, and the owner was warned of the potential risk.
- 9. Further investigation CT imaging • Head – revealed the following changes o The right frontal sinus is fluid filled and the overlying frontal bone is thinned at its rostral limit, axial to the zygomatic process of the frontal bone. o There is mild swelling of the soft tissues dorsal to the zygomatic arch on the right. o The majority of the right nasal cavity is filled with contrast-enhancing soft tissue. o There is evidence of turbinate destruction, and partial lysis of the right naso-orbital wall (likely involving the lacrimal, palatine and maxillary bones). o Gas pockets are visible within the soft tissues of both orbits (incidental). o The right mandibular and right medial retropharyngeal lymph nodes are enlarged (7 mm and 8-10 mm respectively). • Thorax – was unremarkable > Test results continued on next page ABOVE: CT images of the skull, viewed using a bone window (A) and a soft-tissue window pre-(B) and post-(C) contrast, immediately rostral to the orbits. The contrast enhancing soft-tissue mass in the right nasal cavity is indicated (A; arrows), as is the bony destruction lateral to the mass (A; arrow head) A C B LEFT: CT image, viewed using a bone window, at the level of the middle of the orbits revealing the fluid containing right frontal sinus (arrow head)
- 10. Further investigation (continued) Rhinoscopy • Retroflexed rhinoscopy: the nasopharynx was slightly irregular with small undulations on the ventral surface • Anterograde rhinoscopy: examination of the left nasal passage revealed a small amount of mucopurulent discharge and slight hyperaemia of the mucosal surfaces. Examination of the right nasal passage revealed: moderate amounts of purulent discharge; very irregular turbinates; and a large, pale, mass-lesion occupying the dorsal and rostral nasal chamber. Cytology • Nasal flush: Scattered neutrophils made up the majority of the cells present. These were very poorly preserved. There were also occasional large squamous epithelial cells, some with Simonsiella bacteria attached. • Nasal biopsy impression smear: Across the smears there were very high numbers of nucleated cells and moderated numbers of erythrocytes. The nucleated cells were predominantly (>90%) neutrophils, which appeared somewhat ragged, with the vast majority of the remainder being ciliated columnar respiratory epithelial cells. These showed moderate cytoplasmic basophilia, anisocytosis and anisokaryosis. There were occasional binucleated examples. Occasional macrophages were also present. No organisms were noted. Comment: Marked neutrophilic inflammation and accompanying dysplasia in the epithelium. The cause for the inflammation is not evident. > Test results continued on next page
- 11. Further investigation (continued) Nasal Histopathology • Right nasal biopsy: Where present, the surface is predominantly covered by pseudostratified, columnar, ciliated, (respiratory) epithelium. Within the propria-submucosa there is patchy oedema and recent haemorrhage; vessels are generally congested and small vessels frequently contain increased numbers of granulocytes. In addition, there is a patchy, moderate to focally marked increase in lymphocytes and plasma cells with moderate infiltration by neutrophils. Portions of turbinate bone are present and appear normal. In one section, there is focal deposition of amorphous to hyaline, birefringent, palely eosinophilic material within the propria-submucosa, but fails to stain with Congo red (collagen). Adjacent to the surface of the sections there are aggregates of neutrophils, admixed with sloughed epithelial cells, free red blood cells and a background of flocculent to wispy, eosinophilic material (mucus). Staining with PAS fails to identify the presence of fungi. A separate section is presented on a second slide, and comprises an aggregate of neutrophils, admixed with free red blood cells, sloughed epithelial cells and abundant finely granular, basophilic material that stains negatively with Gram, the appearance of which is suspicious of Gram-negative bacteria. Staining with PAS fails to identify the presence of fungi. • Left nasal biopsy: The sections comprise portions of nasal turbinate that are covered by respiratory epithelium. There is some oedema of the propria-submucosa and small vessels are generally congested; there is patchy, mild infiltration of the propria-submucosa by neutrophils and there are focal areas of deposition of a fibrillar, eosinophilic, birefringent extracellular matrix that fails to stain with Congo red (collagen). The fragments comprise small portions of nasal turbinate; portions of squamous epithelium; aggregates of neutrophils that are admixed with free red blood cells, and flocculent, eosinophilic material. Staining with PAS fails to identify the presence of fungi. Comment: Within the sections collected from the right nasal cavity there is a patchy, moderate to focally severe rhinitis, comprising lymphocytes, plasma cells and neutrophils, with evidence of exudation and in one section, a suspicion of Gram-negative bacteria. Within the sections collected from the left nasal cavity there is a patchy, mild neutrophilic rhinitis. Within the sections collected from both nasal cavities there are areas of deposition of collagen (fibrosis). There is no evidence of neoplasia or fungal infection in the sections examined. > Test results continued on next page
- 12. Further investigation (continued) Nasal biopsy culture (left and right) Fungal culture: negative Extended bacterial culture (aerobic and anaerobic): negative Serum protein electrophoresis Revealed a polyclonal gammopathy Abdominal ultrasound Bilateral renal changes: o Shrunken size (right kidney 27mm in length; left kidney 37mm in length) o Irregular outline (considered secondary to multiple chronic renal infarcts) o Cortices were very hyperechoic, with poor corticomedullary differentiation o Faint corticomedullary rim sign QUESTION 5: What do you think is going on? What do you want to do next? > Go to next page for answers
- 13. QUESTION 5: What do you think is going on? What do you want to do next? ANSWER: Follow-up conclusions, treatment & outcome Follow-up conclusions • Destructive, invasive nasal mass – biopsy revealed suspected suppurative neutrophilic rhinitis / turbinate osteomyelitis, but culture was negative • Chronic kidney disease – IRIS stage II; non-hypertensive; borderline proteinuric Secondary bacterial infection is not uncommon during nasal disease – due to altered production and flow of mucus. This explains the, often partial, response to antimicrobials – but the frequent recurrence when the antimicrobials are discontinued. Combined with the low likelihood of primary nasal turbinate osteomyelitis, high likelihood of nasal neoplasia in an older cat with nasal signs, and (unpublished) data that indicate ~ 1 in 3-4 companion animals with nasal biopsies (performed by specialists) require repeat nasal biopsy in order to confirm the diagnosis, a missed diagnosis of nasal neoplasia could not be ruled out. Further investigation (i.e. repeat biopsy) was declined by the client at that time. The negative bacterial culture could have been due to the recent antimicrobials, and the lack of response due to the shortness of the course administered. > Answer continued on next page
- 14. QUESTION 5: What do you think is going on? What do you want to do next? ANSWER: Treatment & outcome Chronic kidney disease likely accounted, at least in part, for the reduced appetite, increased thirst and weight loss. They were managed with a renal support diet and monitored – as per the IRIS guidelines (www.iris-kidney.com) The localised nasal infection may have also contributed to the reduced appetite. They were treated with a prolonged (12 week) course of amoxicillin-clavulanate (12mg/kg; q8hrs) – for presumed osteomyelitis. The facial swelling resolved and the sneezing ceased. Repeat imaging (2.5 months after the initial investigation) revealed absence of the mass, resolution of the fluid accumulations, and normal draining lymph nodes. Nasal biopsy histology was consistent with chronic lymphoplasmacytic rhinitis. Blood analysis revealed a resolution of the neutrophilia, an increase in the haematocrit, a gradual reduction in the hyperglobulinaemia, and a gradual progression of the azotaemia (into IRIS grade III). Clinical signs did not recur following completion of the antimicrobial course.