Micro Minerals
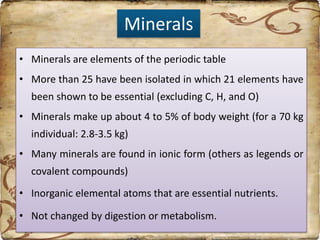
Minerals are essential nutrients that are found in ionic form or as covalent compounds. They make up about 4-5% of body weight and can be categorized as macrominerals or microminerals based on their daily requirements. Iron, zinc, iodine, selenium, copper, manganese, fluoride, chromium, molybdenum, and cobalt are important microminerals. Minerals are involved in many critical functions like oxygen transport, energy production, bone formation, and acting as cofactors for enzymes. Factors like diet, absorption mechanisms, and physiological state can impact an individual's mineral requirements.