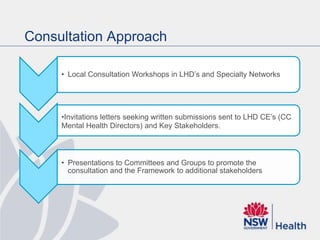
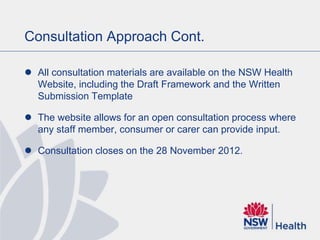
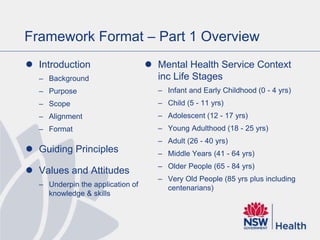
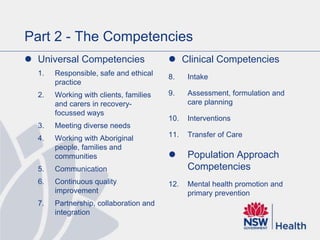
This document outlines a draft NSW Mental Health Services Competency Framework that is being developed to provide a coordinated approach to developing the knowledge and skills of NSW public sector mental health professionals. It provides background on the framework's development, describes its key parts and format, and poses a series of consultation questions. The framework aims to enhance service provision across the lifespan from infant to older adults. It includes universal competencies, clinical competencies, and a population approach competency. Local consultation workshops and an online submission process are being used to gather input on the draft framework.