Mandibular fracture
- 2. OUTLINE • INTRODUCTION • CLASSIFICATION • AETIOLOGY • EPIDEMIOLOGY • SIGNS & SYMPTOMS • INVESTIGATION • MANAGEMENT
- 3. INTRODUCTION • Fracture of the mandible occurs more frequently than that of any other facial skeleton. • It is the one serious facial bone injury that the average practicing dental surgeon may expect to encounter, albeit on rare occasions, at his surgery. • It is also a facial fracture which he may have the misfortune to cause as a complication of tooth extraction. • Broadly divided into: 1. Fractures with no gross communition of the bone and without significant loss of hard and soft tissues 2. Fractures with gross communition of the bone and with extensive loss of both hard and soft tissues.
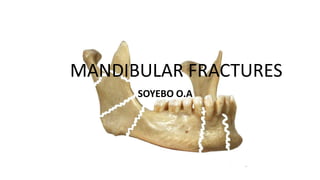
- 4. ANATOMY • Lower jaw bone • U shaped body • 2 vertically directed rami • Condylar process • Coronoid process • Oblique line • Mental foramen
- 5. INTERNAL ANATOMY • • • • • Mandibular foramen Lingula Pterygoid fovea Mylohyoid line Fossae • Submandibular • Sublingual • Digastric • Mental spines • Genioglossus • Geniohyoid
- 6. MUSCULATURE: jaw elevators • Masseter muscle: from zygoma to angle and ramus • Temporalis muscle: from infratemporal fossa to coronoid and ramus. • Medial pterygoid muscle: medial pterygoid plate and pyramidal process into the lower mandible.
- 7. MUSCULATURE: jaw depressors • Lateral pterygoid muscle: lateral pterygoid plate to condylar neck and TMJ capsule • Mylohyoid muscle: Mylohyoid line to body of hyoid • Digastric muscle: mastoid notch to digastric fossa • Geniohyoid muscle: inferior genial tubercle to anterior hyoid bone
- 8. INNERVATION • CN3; mandibular nerve through the foramen ovale • Inferior alveolar nerve through the mandibular foramen • Inferior dental plexus • Mental nerve through the mental foramen.
- 9. BLOOD SUPPLY • Internal maxillary artery • Inferior alveolar artery • Mental artery
- 10. CLASSIFICATION OF FRACTURES • Type of fracture • Site of fracture • Cause of fracture
- 11. TYPE OF FRACTURE • Simple • Includes a closed linear fractures of the condyle, coronoid, ramus and edentulous body of the mandible. • Compound • Fractures of tooth bearing portions of the mandible, into d mouth via the periodontal membrane and at times through the overlying skin. • Communited • Usually compound fractures characterized by fragmentation of bone • Pathological • Results from an already weakened mandible by pathological conditions.
- 13. SITE OF FRACTURE • Dentoalveolar • Condyle • Coronoid • Ramus • Angle • Body (molar and premolar areas) • Parasymphysis • Symphysis
- 14. SITE OF FRACTURE A- CONDYLAR B- CORONOID C-RAMUS D- ANGLE E- BODY(MOLAR PREMOLAR AREAS F- PARASYMPHYSIS G- SYMPHYSIS H-DENTO-ALVEOLAR
- 15. CAUSE OF FRACTURE • Direct violence • Indirect violence • Excessive muscular contraction • Fracture of the coronoid process because of sudden reflex contracture of the temporalis muscle.
- 16. PATTERN OF FRACTURE • Unilateral fracture • Bilateral fracture • Multiple fracture • Communited fracture
- 17. AETIOLOGY • Road traffic accidents • Interpersonal violence • Contact sports • Industrial trauma • Falls
- 18. EPIDEMIOLOGY • The mandible is one of the most commonly fractured bones of the face and this is directly related to its prominent and exposed position. • Oikarinen and Lindqvist (1975) studied 729 patients with multiple injuries sustained in RTA. The most common facial fractures were in the mandible. • • • • Mandible (61%) Maxilla (46%) Zygoma(27%) Nasal Bone (19%)
- 19. • Studies have shown that the incidence of mandible fractures are influenced by various etiological factors e.g. • • • • Geography Social trends Road traffic legislations Seasons
- 20. • Site of Fracture: Oikarinen and Malmstrom (1969) analyzed 600 mandible fractures. On analysis the following results were obtained: • • • • • • • Body of mandible (33.6%) Sub- condylar area(33.4%) Angle (17.4%) Dentoalveolar (6.7%) Ramus (5.4%) Symphyseal 2.9% Coronoid 1.3%
- 21. • Even though the body of the mandible has the highest incidence when it comes to mandibular fracture, the condyle remains the commonest site for mandibular fracture
- 22. SIGNS AND SYMPTOMS • GENERAL • SPECIFIC
- 23. GENERAL SIGNS AND SYMPTOMS • Swelling • Pain • Drooling • Tenderness • Bony discontinuity • Lacerations • Limitation in mouth opening • Ecchymosis • Fractured, subluxed, luxated teeth. • Bleeding from the mouth.
- 24. SPECIFIC SIGNS AND SYMPTOMS • DENTOALVEOLAR FRACTURES • • • • • Lip bruises and laceration Step deformity Bony discontinuity Fracture, luxation or subluxation of teeth Laceration of the gingivae • FRACTURE OF THE BODY • • • • • • Swelling pain Tenderness Step deformity Anaesthesia or paraesthesia of the lip Intra oral hemorrhage • SYMPHYSEAL/PARASYMPHYSEAL FRACTURES • • • • Tenderness Sublingual haematoma Loss of tongue control soft tissue injury to the chin and lower lip
- 25. • FRACTURE OF THE RAMUS • • • • Swelling Ecchymosis Pain Trismus • FRACTURE OF THE ANGLE • • • • • • • Swelling Posterior gag Deranged occlusion Anaesthesia or paraesthesia of lower lip Haematoma Step deformity behind the last molar tooth Tenderness
- 26. • CORONOID FRACTURE • • • • Tenderness over the anterior part of the tragus Haematoma Painful limitation of movement Protrusion of mandible may be present. • SYMPHYSEAL/PARASYMPHESEAL FRACTURES • • • • • • Tenderness pain Step deformity Sublingual haematoma Loss of tongue control May have soft tissue injury to the chin and lower lip
- 27. • CONDYLAR FRACTURE (unilateral/bilateral and Intracapsular/extracapsular) • Unilateral condylar fractures • • • • • • • • Swelling over the TMJ Hemorrhage from ear on the affected side Battle’s sign Locked mandible Hollow over the condylar region after edema has subsided rarely, Paraesthesia of lower lip Deviation to the affected side upon opening Painful limitation of movement
- 28. • Bilateral condylar fractures • • • • Same as above Limitation in mouth opening Restricted mandibular movement Anterior open bite
- 29. INVESTIGATION • Treatment plan for mandibular fractures is very dependent on precise radiological diagnosis • RADIOGRAPHS • Essential radiographs • Extra-oral radiographs • Intra-oral radiographs • Desirable radiographs
- 30. Essential Extra-oral Radiographs • Oblique lateral radiographs (left and right) • Fracture of body proximal to canine region • Fractures of angle, ramus and condylar region
- 31. • Posterior-anterior view • Shows displacement of fractures in the ramus, angle, body • Rotated posterior-anterior view • Fractures between Symphysis and canine region
- 32. • Reverse Towne’s view • Ideal for showing lateral or medial condylar displacement
- 33. Essential Intra-oral Radiographs • Periapical radiographs: • Association of tooth to line of fracture • Existing pathology related to tooth in line of fracture • Fracture of tooth in line of mandibular fracture • Occlusal radiographs: • Association of root of tooth to line of fracture
- 34. Desirable Radiographs • Panoramic tomography • represents the best single overall view of the mandible especially the condyles • Standard linear tomography • Computed tomography (CT)
- 35. MANAGEMENT • Airway • • • • • • • • • • • Tongue falling back Blood clots Fractured teeth segments Broken fillings Dentures Hemorrhage Soft tissue lacerations Support of bone fragments Pain control Infection control e.g. compound fractures Food and Fluid
- 36. DEFINITIVE TREATMENT • Reduction • Restoration of a functional alignment of the bone fragments • Use of occlusion 1. Open reduction 2. Closed reduction • Immobilization • To allow bone healing • Through fixation of fracture line 1. Rigid 2. Non-rigid
- 37. BONE HEALING • Bone healing is altered by types of fixation and mobility of the fracture site in relation to function • Primary bone healing • Secondary bone healing
- 38. Bone Healing • Primary bone healing: • No fracture callus forms • Heals by a process of 1. Haversian remodeling directly across the fracture site if no gap exists (Contact healing), or 2. Deposition of lamellar bone if small gaps exist (Gap healing) • Requires absolute rigid fixation with minimal gaps
- 39. Bone Healing Contact Healing Gap Healing
- 40. Bone Healing • Secondary bone healing: • Bony callus forms across fracture site to aid in stability and immobilization • Occurs when there is mobility around the fracture site
- 41. Bone Healing • Secondary bone healing involves the formation of a sub periosteal hematoma, granulation tissue, then a thin layer of bone forms by membranous ossification. Hyaline cartilage is deposited, replaced by woven bone and remodels into mature lamellar bone
- 42. Bone Healing
- 43. TEETH IN LINE OF FRACTURE • Teeth in line of fracture are a potential impediment to healing for the following reasons 1. The fracture is compound into the mouth via the opened periodontal membrane 2. The tooth may be damaged structurally or loose its blood supply as a result of the trauma so that the pulp subsequently becomes necrotic 3. The tooth may be affected by some pre-existing pathological process • Indications for removal • Absolute • Relative
- 44. Absolute indications • Longitudinal fracture involving the root • Dislocation or subluxation of tooth from socket • Presence of periapical infection • Infected fracture line • Acute pericoronitis
- 45. Relative indications • Functionless tooth which would eventually be removed electively • Advanced caries • Advanced periodontal disease • Teeth involved in untreated fractures presenting more than 3days after injury
- 46. Management of teeth retained in fracture line • Good quality intra-oral periapical radiograph • Appropriate antibiotic therapy • Splinting of tooth if mobile • Endodontic therapy if pulp is exposed • Immediate extraction if fracture becomes infected
- 47. IMMOBILIZATION • The period of stable fixation required to ensure full restoration of function varies according to: 1. Site of fracture 2. Presence of retained teeth in the line of fracture 3. Age of the patient 4. Presence or absence of infection
- 48. • A simple guide to time of immobilization for fractures of the tooth bearing area of the mandible is as follows: Young adult with Fracture of angle Receiving Early treatment In which Tooth removed from fracture line 3 weeks
- 49. • If: a) Tooth retained in fracture line: add 1 week b) Fracture at Symphysis: add 1 week c) Age 40yrs and above: add 1 or 2 weeks d) Children and adolescent: subtract 1 week
- 50. METHODS OF IMMOBILIZATION • Osteosynthesis without intermaxillary fixation 1. 2. 3. 4. Non-compression small plates Compression plates Mini plates Lag screws
- 51. • Intermaxillary fixation 1. Bonded brackets 2. Dental wiring 1. Direct 2. Eyelet 3. Arch bars 4. Cap splints
- 52. • Intermaxillary fixation with Osteosynthesis 1. 2. 3. 4. 5. Trans osseous wiring Circumferential wiring External pin fixation Bone clamps Transfixation with kirschner wires
- 53. CLOSED REDUCTION • Fracture reduction that involves techniques of not opening the skin or mucosa covering the fracture site • Fracture site heals by secondary bone healing • This is also a form of non-rigid fixation
- 54. • “If the principle of using the simplest method to achieve optimal results is to be followed, the use of closed reduction for mandibular fractures should be widely used” Peterson’s Principle of Oral and Maxillofacial Surgery 2nd edition • INDICATIONS 1. Nondisplaced favorable fractures 2. Mandibular fractures in children with developing dentition 3. Condylar fractures
- 55. • CONTRAINDICATIONS: 1. Alcoholics 2. Seizure disorder 3. Mental retardation 4. Nutritional concerns 5. Respiratory diseases (COPD) • Unfavorable fractures
- 56. • ADVANTAGES 1. Low cost 2. Short procedure time 3. Can be done in clinical setting with local anesthesia or sedation 4. Easy procedure
- 57. • DISADVANTAGES 1. Not absolute stability (secondary bone healing) 2. Oral hygiene difficult 3. Possible TMJ sequelae a) Muscular atrophy/stiffness b) Decrease range of motion
- 58. • TECHNIQUES: 1. Arch bars – Erich arch bars 2. Ivy loops 3. Essig Wire 4. Intermaxillary fixation screws 5. Splints 6. Bridal wires
- 60. OPEN REDUCTION • Implies the opening of skin or mucosa to visualize the fracture and reduction of the fracture Can be used for manipulation of fracture only Can be used for the non-rigid and rigid fixation of the fracture • INDICATIONS Unfavorable/unstable mandibular fractures Fractures of an edentulous mandible fracture with severe displacement Delayed treatment with interposition of soft tissue that prevents closed reduction techniques to re-approximate the fragments
- 62. Open reduction/ non rigid
- 63. SPECIAL CONSIDERATIONS • Edentulous mandible • Mandible in children
- 64. Mandibular Fractures in children • Mandible is resilient at this period • Line between cortex and medulla is less well defined • High ratio of bone to teeth substance • Factors to consider in treating fractures in children • Interference with growth potential • Fixation in deciduous/mixed dentition • Unerupted teeth
- 65. Fracture of Edentulous mandible • Influencing factors: 1. Decreased inferior alveolar artery (centrifugal) blood flow 2. Dependent on periosteal (centripetal) blood flow 3. Medical conditions that delay healing 4. Decreased ability to heal with age 5. Altered physical characteristics following tooth loss
- 66. • Methods of immobilization: • Direct Osteosynthesis 1. Bone plates 2. Transosseous wiring 3. Circumferential wiring • Indirect skeletal fixation 1. Pin fixation 2. Bone clamps • Intermaxillary fixation using gunning type splints 1. Used alone 2. Combined with other techniques
- 67. COMPLICATIONS • Misapplied fixation • Infection • TMJ ankylosis • Nerve damage • Displaced teeth • Gingival and periodontal complications
- 68. • Malunion • Delayed union/Non union • Inadequate immobilization, fracture alignment • Interposition of soft tissue or foreign body • Incorrect technique • Limitation in mouth opening • Scar formation
- 69. CONCLUSION • An adequate knowledge of the diagnosis and management of various types of mandibular fracture is needed so as to provide the desired treatment in order to prevent unfavorable and adverse complications.
