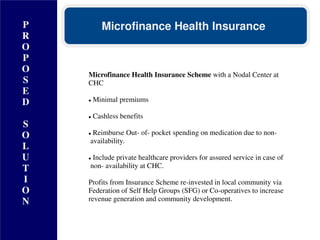
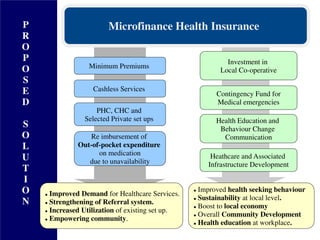
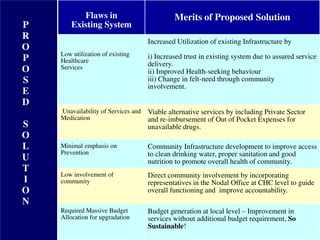
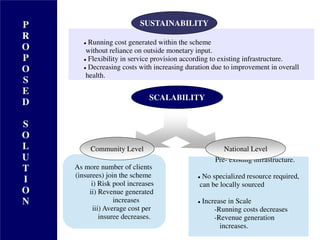
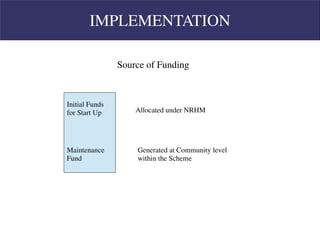
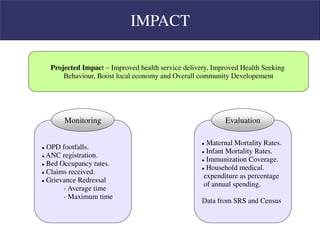
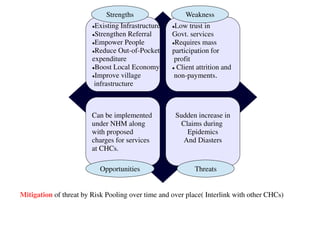
The document proposes a microfinance health insurance scheme to improve access to quality primary healthcare in rural communities. It would establish a nodal center at community health centers to provide minimum premiums, cashless benefits, and reimbursement for out-of-pocket medical expenses. Profits would be reinvested in self-help groups and cooperatives to generate revenue and develop local infrastructure. This aims to increase utilization of existing healthcare services, strengthen referrals, empower communities, and boost the local economy through a sustainable community-level solution.




![References
Raykumar P et al
Health care seeking and treatment cost in a rural community of West Bengal, India ,
[theHealth 2012; 3(3): 67-70]
Mandal S, Kanjilal B, Peters DH, Lucas H.
Catastrophic out-of-pocket pay-ment for health care and its impact on households:
Experience from West Bengal, India.
Ray TK, Pandav CS, Anand K, Kapoor SK, Dwivedi SN.
Out-of-pocket expenditure on healthcare in a north Indian village.
[Natl Med J India. 2002;15:257-60.]
Rose Ann Dominic et al
Health seeking behavior of rural adults.
[NUJHS Vol. 3, No.3, September 2013, ISSN 2249-7110]](https://image.slidesharecdn.com/2-mamc-doctors-1378421449-130906034940-/85/MAMC-DOCTORS-20-320.jpg)
![References
Ghosh et al
Factors affecting the healthcare seeking behaviour of mothers regarding their children in
a rural community of Darjeeling district, West Bengal.
[International Journal of Medicine and Public Health,Jan-Mar 2013,Vol 3,Issue 1 ]
Programme Evaluation Organisation, Planning Commission,Government of India
Evaluation Study of National Rural Health Mission (NRHM) in 7 States [2011]](https://image.slidesharecdn.com/2-mamc-doctors-1378421449-130906034940-/85/MAMC-DOCTORS-21-320.jpg)