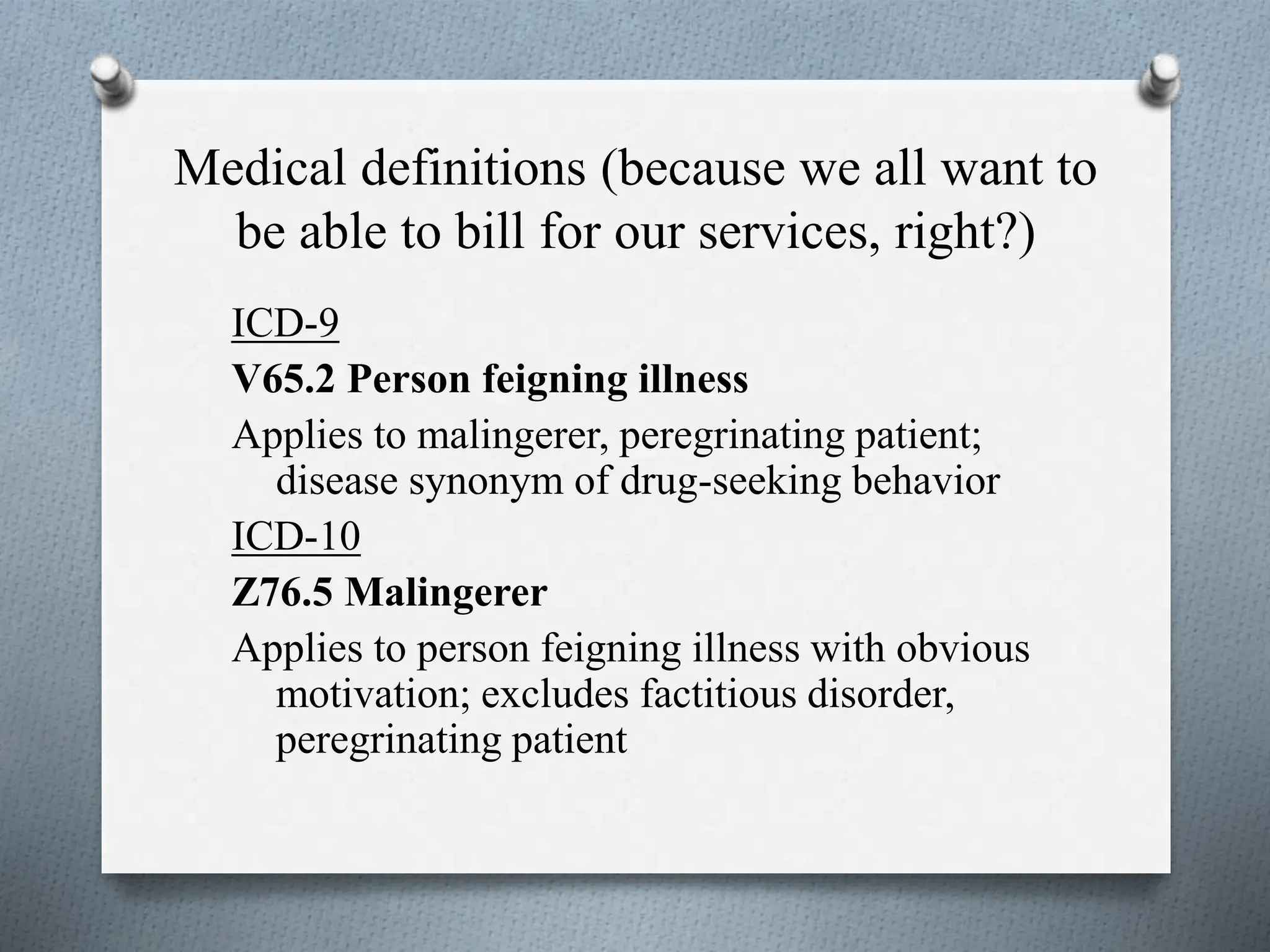
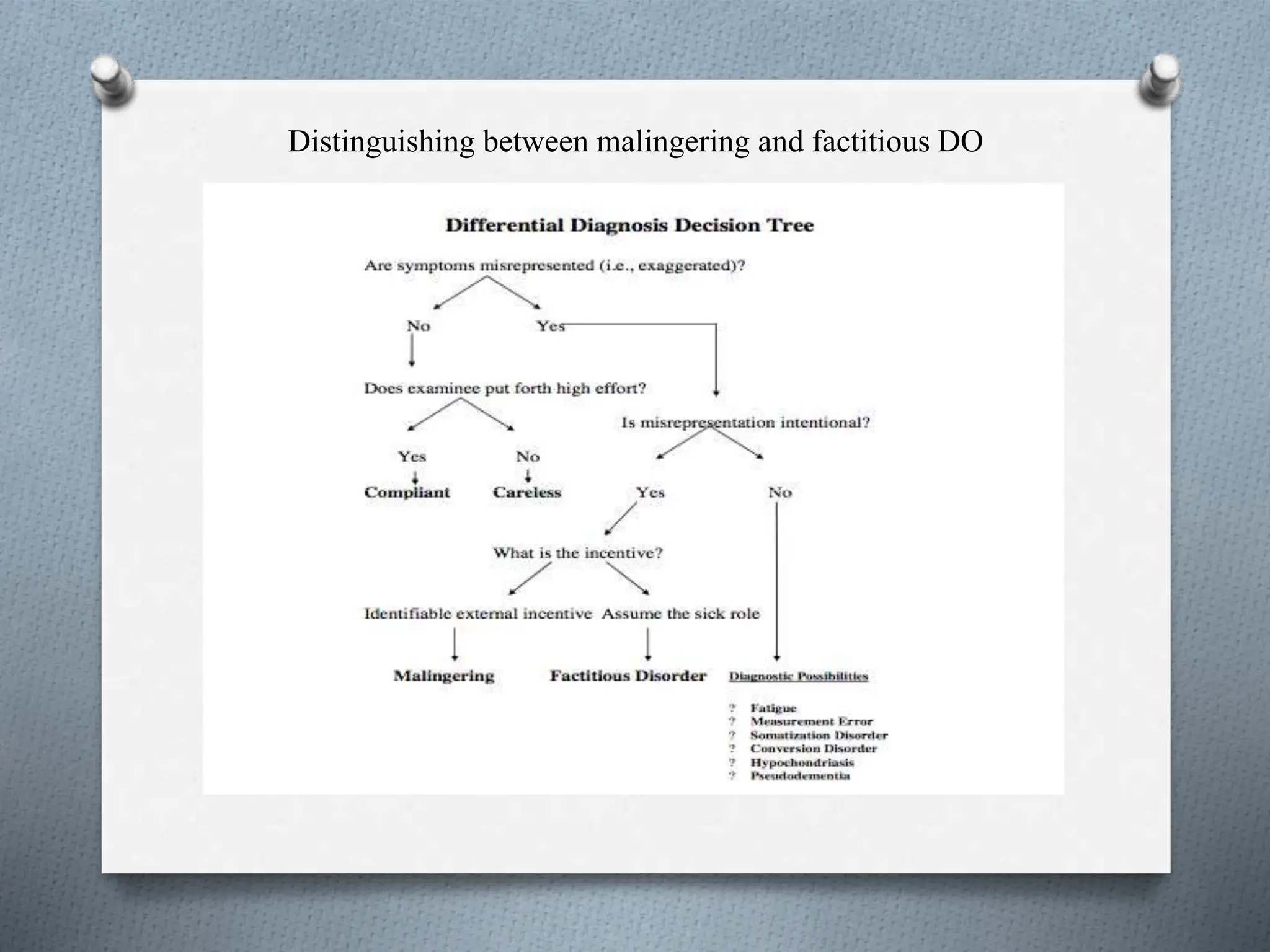
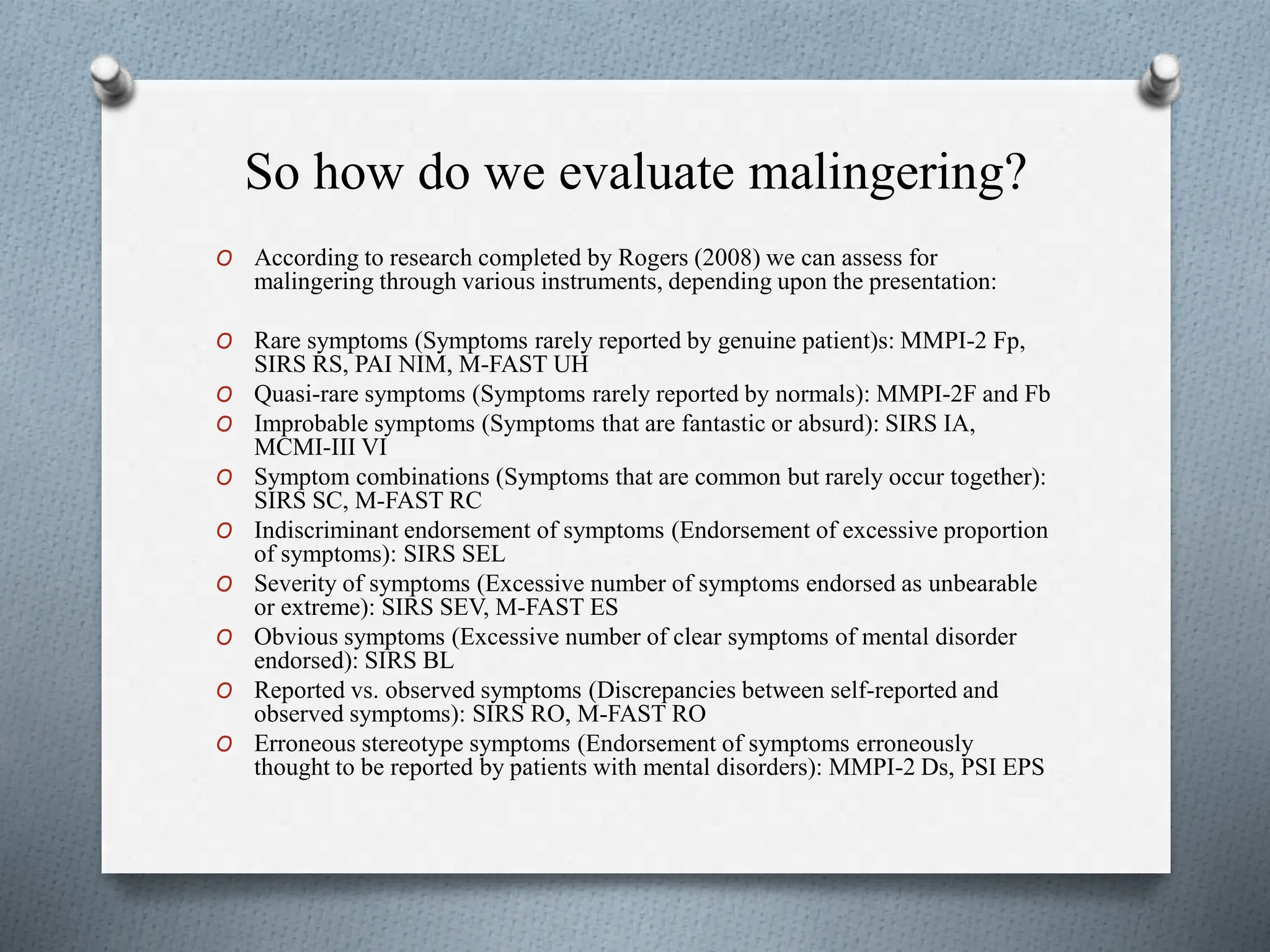
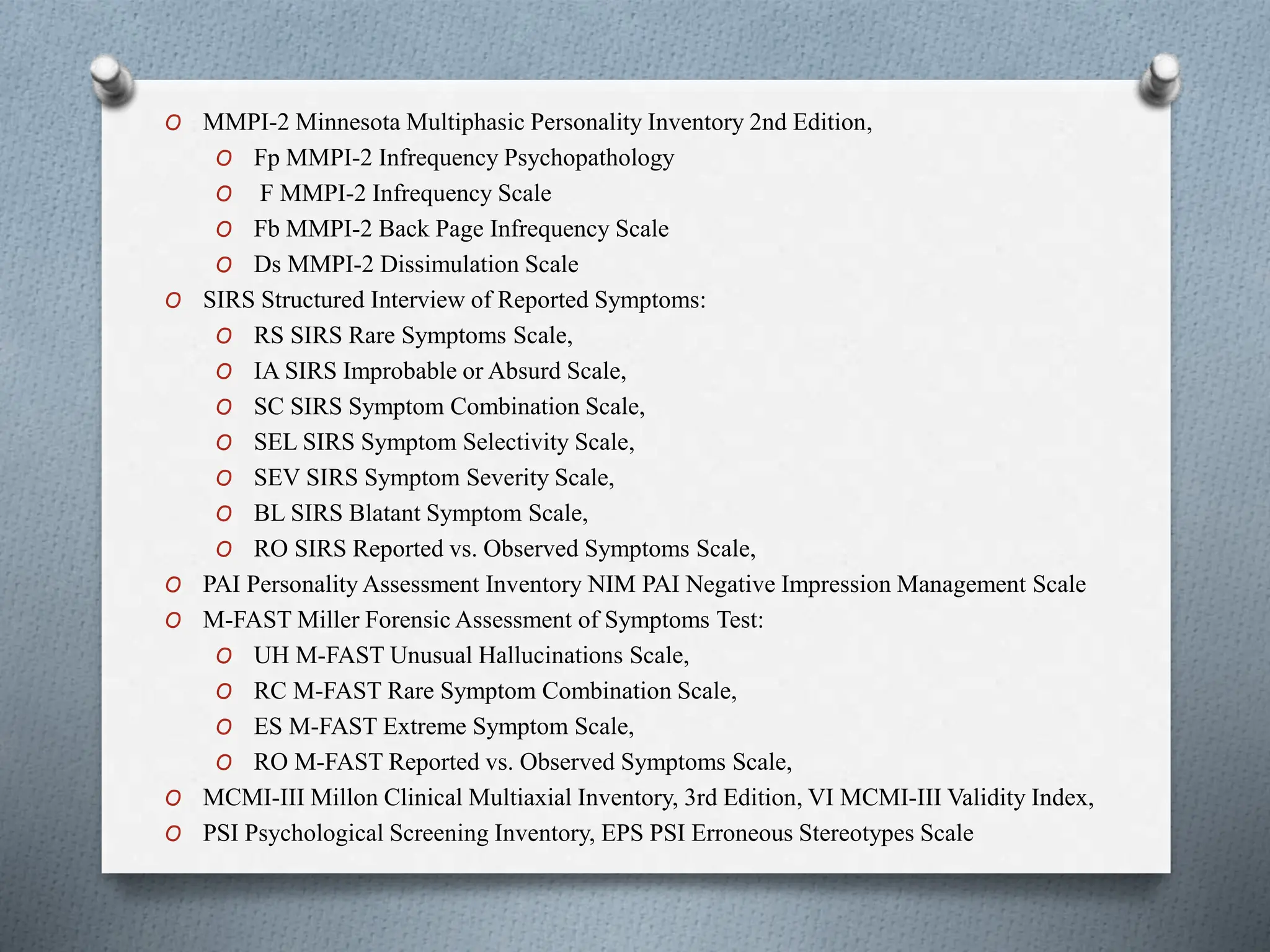
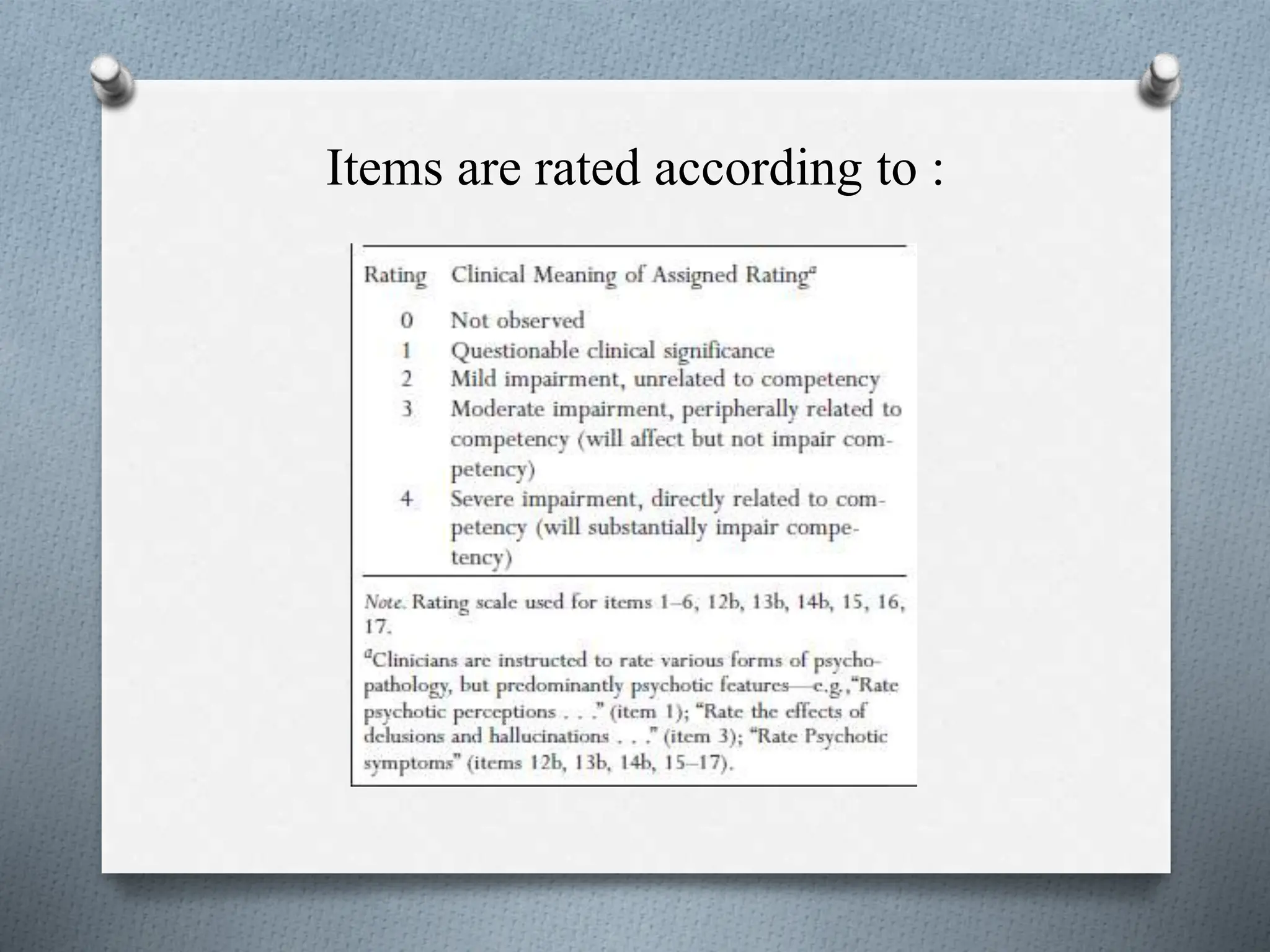
The document reviews malingering, defining it as the intentional exaggeration or fabrication of symptoms for external gain, and contrasts it with other disorders like factitious disorder. It discusses various assessments and instruments used to evaluate malingering in both civil and criminal contexts, highlighting specific symptoms and their associations. Additionally, the document outlines the importance of distinguishing true malingering from genuine psychological issues, referencing multiple studies and tools for effective detection.