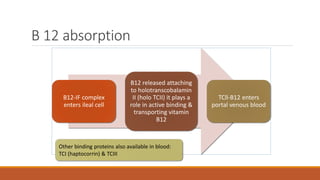
Megaloblastic anemia is characterized by large, immature red blood cells caused by vitamin B12 or folate deficiency. It is seen in specific populations like the elderly, alcoholics, and those with gastric issues or taking certain medications. Pernicious anemia is a type of megaloblastic anemia caused by lack of intrinsic factor leading to vitamin B12 deficiency. Diagnosis involves blood tests of vitamin B12, folate, homocysteine and methylmalonic acid levels. Treatment is vitamin B12 injections or high oral doses. Medical nutrition therapy focuses on vitamin B12 and folate rich foods. Other nutritional anemias include copper deficiency, protein-energy malnutrition, and vitamin E or pyrid