Lymphatic Filariasis.pptx
- 1. Lymphatic Filariasis Dr .C.SASHIDHARAN Assistant Professor Dept of Community Medicine MAPIMS
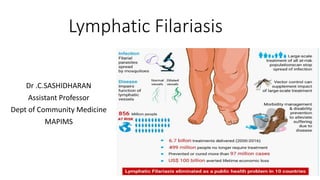
- 2. Introduction • Lymphatic filariasis, • Commonly known as elephantiasis • A neglected tropical disease. • Infection occurs when filarial parasites are transmitted to humans through mosquitoes. • Infection is usually acquired in childhood causing hidden damage to the lymphatic system.
- 3. Global Burden • Currently, 1.4 billion people in 73 countries are living in areas that require preventive chemotherapy to stop the spread of infection. • Approximately 80% of these people are living in the following 10 countries: Angola, Cameroon, Democratic Republic of the Congo, India, Indonesia, Mozambique, Myanmar, Nigeria and the United Republic of Tanzania.
- 4. The disease manifestations range from none to both acute and chronic manifestations • Lymphangitis, lymphadenitis, • elephantiasis of genitals, legs and arms or • as a hypersensitivity state such as tropical pulmonary eosinophilia or • as an atypical form such as filarial arthritis. • Though not fatal, the disease is responsible for considerable suffering, deformity and disability.
- 5. Epidemiological determinants Agent factors: There are at least 8 species of filarial parasites that are specific to man.
- 6. Causative Organism Vectors Diseases produced Lymphatic W.Bancrofti culex Lym filariasis Brugia malayi Mansonia Lym filariasis B.timori Anopheles Mansonia Lym filariasis Sub cutaneous Onchocerca volvulus, Simulum flies Sub cut nodules River blindness Loa loa Chrysopes Sub cut nodule Mansonella streptocerca Culicoides Rarely serous Mansonella perstans, Culicoides Rarely M.ozzardi. culicoides Rarely
- 7. • Lymphatic filariasis is caused by infection with parasites classified as nematodes (roundworms) of the family Filariodidea 1. Wuchereria bancrofti, which is responsible for 90% of the cases 2. Brugia malayi, which causes most of the remainder of the cases 3. Brugia timori, which also causes the disease.
- 9. PERIODICITY: The Mf of W. bancrofti and B.malayi occurring in .India display a nocturnal periodicity. This is a biological adaptation to the nocturnal habits of the vector mosquitoes The maximum density in blood is reported between 10 pm and 2 am When the sleeping habits of the host are altered, a reversal in periodicity has been observed.
- 10. Wuchereria bancrofti • the causative organism for filaria transmitted by the ubiquitous vector, Culex quinquefasciatus, • has been the most predominant infection contributing to 99.4% of the problem in the country. • Although the vector species breeds preferably in dirty and polluted water, it can also breed in clear water in the absence of polluted water. • The infection is prevalent in both urban and rural areas
- 11. Brugia malayi • mainly rural areas due to peculiar breeding habits of the vector associated with floating vegetation. • Mansonia (Mansonioides) annulifera- principal vector M.(M).uniformis is the secondary vector for transmission • The breeding of these mosquitoes is associated with aquatic plants such as Pistia stratiotes. In the absence of these plants, the vectors cannot breed. • The vectorial role of M. (M). indiana is very limited due to its low density.
- 12. • Both W. bancrofti and B. malayi infections in mainland India exhibit nocturnal periodicity of microfilaraemia.
- 13. Life cycle • Man is the definitive host and mosquito the intermediate host of Bancroftian and Brugian filariasis. • The adults worms are usually found in the lymphatic system of man. The males are about 40 mm long and the females 50 to 100 mm long. • The females are viviparous
- 14. • Adult worms lodge in the lymphatic system and disrupt the immune system. • The worms can live for an average of 6–8 years and, during their life time, produce millions of microfilariae (immature larvae) that circulate in the blood.
- 15. LIFE CYCLE OF FILARIAL PARASITE exsheathing
- 16. RESERVOIR OF INFECTION • Although filarial infections occur in animals. Human filariasis is not usually a zoonosis • Animal reservoirs of Brugia, present in monkeys, cats and dogs; these animals are believed to acquire their infections from man. and they are not regarded as important sources of infection to man
- 17. Host factors •Man is the natural host •Age: All ages are susceptible to infection • infected early in childhood microfilaremia peaks between 15-20years plateaus in adult life. declines in middle and old age
- 18. • Sex : Equally susceptible • Immunity: Man may develop resistance to infection only after many years of exposure • SOCIAL FACTORS : Lymphatic filariasis is often associated with urbanization, industrialization, migration of people, illiteracy, poverty and poor sanitation
- 19. Environmental factors Climate: • It influences the breeding of mosquitoes, their longevity and also determines the development of the parasite in the insect vector • Tropical climate favorable • Humidity: 80% • Temperature: 20- 40 degrees
- 20. • DRAINAGE: lymphatic filariasis is associated with bad drainage. The vectors breed profusely in polluted water • Town Planning : The common breeding places are cesspools, sokage pits. ill-maintained drains, septic tanks, open ditches
- 21. Vectors of lymphatic filariasis • The main vectors in India are : C. quinquefasciatus(C. fatigans) for Bancroftian filariasis, • Monsonia (mansonoides) mosquitoes (e.g.., M.annulifers and M.Uniformis) for Brugian filariasis.
- 22. MODE OF TRANSMISSION Bite of infected mosquitoes (culex quinquefasciatus) INCUBATION PERIOD Pre patent period- Time interval between inoculation of the infective microfilaria and the first appearance of microfilaria in peripheral blood
- 23. Extrinsic incubation period- Time taken from the entry of microfilaria in mosquito till the development of infective 3rd stage larva Clinical incubation period- Time interval from invasion of microfilaria till the development of clinical manifestations i.e.,8 to 16months
- 24. DISEASE MANIFESTATION Divided into 2 distinct clinical types: 1)Lymphatic filariasis caused by the parasite in the lymphatic system 2)Occult Filariasis caused by immune hyperresponsiveness of the human host(eg. Tropical pulomonary eosinophilia)
- 25. LYMPHATIC FILARIASIS 1. Asymptomatic amicrofilaraemia - does not show Mf or clinical manifestations of the disease. 2. Asymptomatic microfilaraemia – asymptomatic but blood is positive for Mf. Important source of infection in the community.
- 26. 3. Stage of acute manifestation – first months and yrs there are recurrent episodes of acute inflammation in the lymph glands and vessels 4. Stage of chronic obstructive lesion – develops 10-15 yrs from the onset of the first acute attack. Due to fibrosis and obstruction of the lymphatic vessels causing permanent structural changes.
- 27. Occult or Cryptic filariasis refers to filarial infections in which the classical clinical manifestations are absent and Mf are not found in the blood . Believed to result from a hypersensitivity reaction to filarial Ag derived from Mf.
- 28. • A definitive diagnosis can be made only by detection of the parasites. • Identification of microfilariae in a blood smear by microscopic examination. • The microfilariae exhibit nocturnal periodicity with surges of circulating microfilariae at night. Blood collection should be done at night to coincide with the appearance of the microfilariae.
- 29. MANAGEMENT Lymphoedema management: In areas with lymphatic filariasis, improving the quality of life by activities such as – -early detection of lymphoedema -caring for the skin by washing -drying the affected limb or area -preventing and treating entry lesions and providing lymph drainage by elevating the limb and exercising
- 31. Guidelines by WHO to manage ADLA (Acute Dermatolymphangioadenitis) : -Treatment for uncomplicated ADLA -Treatment for complicated ADLA
- 32. • Treatment for uncomplicated ADLA Give analgesic- paracetamol (1gm 3times a day) Give oral antibiotic-amoxicillin (1.5gm in 3doses) or oral penicillin should be given for 8 days Clean the limb with antiseptic
- 33. Any superficial infection antibiotic or antifungal cream should be applied Give advice on prevention of lymph edema DO NOT GIVE Anti filarial medicine Home management and follow up after 2 days
- 34. Treatment for complicated ADLA Refer the patient to physician immediately Antibiotic treatment-iv penicillin G 5million units or procaine benzyl penicillin 2million units Give analgesic or antipyretic Do not give anti filarial medicine during acute attacks.
- 36. Antifilarial treatment • All people with filariasis who are positive in the immunochromatographic test or have microfilaraemia should receive anti-filarial drug treatment to eliminate microfilariae
- 37. Regimens • (i) a single dose of a combination of albendazole (400 mg) with ivermectin (150–200 µg/kg) in areas where onchocerciasis is co-endemic • In areas where onchocerciasis is non co-endemic, either (ii) a single dose of a combination albendazole (400 mg) plus diethylcarbamazine (6 mg/kg) or (iii) diethylcarbamazine 6 mg/kg alone for 12 days
- 38. FILARIA SURVEY Mass blood survey- • Thick film- Giemsa stained • Membrane filter concentration- for detecting low density microfilaraemia in blood • DEC provocation test- Mf can be induced to appear in blood in the day time by administering DEC 100mg orally. Blood may be examined 1hr after the administration.
- 39. 2. Clinical survey- examined for clinical manifestations 3. Serological tests- detection of parasite antigens in patients blood or urine, CFT 4. Imaging - CT,MRI may reveal "Filarial Dance Sign" in Chylus fluid. X- ray can show calcified adult worm in lymphatics
- 40. 5. Xenodiagnosis: the mosquitoes are allowed to feed on the patient and then dissected 2 weeks later 6. Epidemiological survey
- 41. Assessment of filaria control programme Clinical parameters- Incidence of acute manifestations Prevalence of chronic manifestations Parasitological parameters- Microfilaria rate Filarial endemicity rate Microfilaria density Average infestation rate
- 42. Entomological parameters- Vector density per 10 man hour catch Percentage of mosquitoes positive for all stages of development Percentage of mosquitoes positive for infective larvae Types of larval breeding places
- 43. Filaria control in the community- Chemotherapy Mass treatment-every member of the community irrespective of infection are treated with DEC Selective treatment-DEC is given to those who are microfilaria positive DEC medicated salt-fortified common salt medicated with 1-4gm DEC per kg is used in endemic areas Ivermectin-oral dose of 20-400micro gm per kg is effective in clearing Mf
- 44. Filaria control in the community- Vector control • Antilarval measures- -Chemical control: mosquito larvicidal oil Pyrosene oil-E Organophosphorous compounds Removal of pistia plant Minor environmental measures
- 45. • Antiadult measures-pyrethrum is used as space spray, • Personal prophylaxis-avoid mosquito bites by using mosquito nets and repellants
- 47. Interrupting transmission • Annual mass administration of a combination of two drugs to entire populations at risk. • Albendazole (400 mg) plus either diethylcarbamazine (6 mg/kg) in areas without onchocerciasis or loiasis, or ivermectin (150–200 µg/kg) in areas where onchocerciasis and lymphatic filariasis are co-endemic
- 49. Previous year questions • Long question : • (1) Discuss the epidemiology, prevention and control of Lymphatic Filariasis. • Short Notes : • (1) Clinical Spectrum of Filariasis • (2) Treatment of Lymphatic Filariasis and mass treatment regimen.
- 50. Thank you