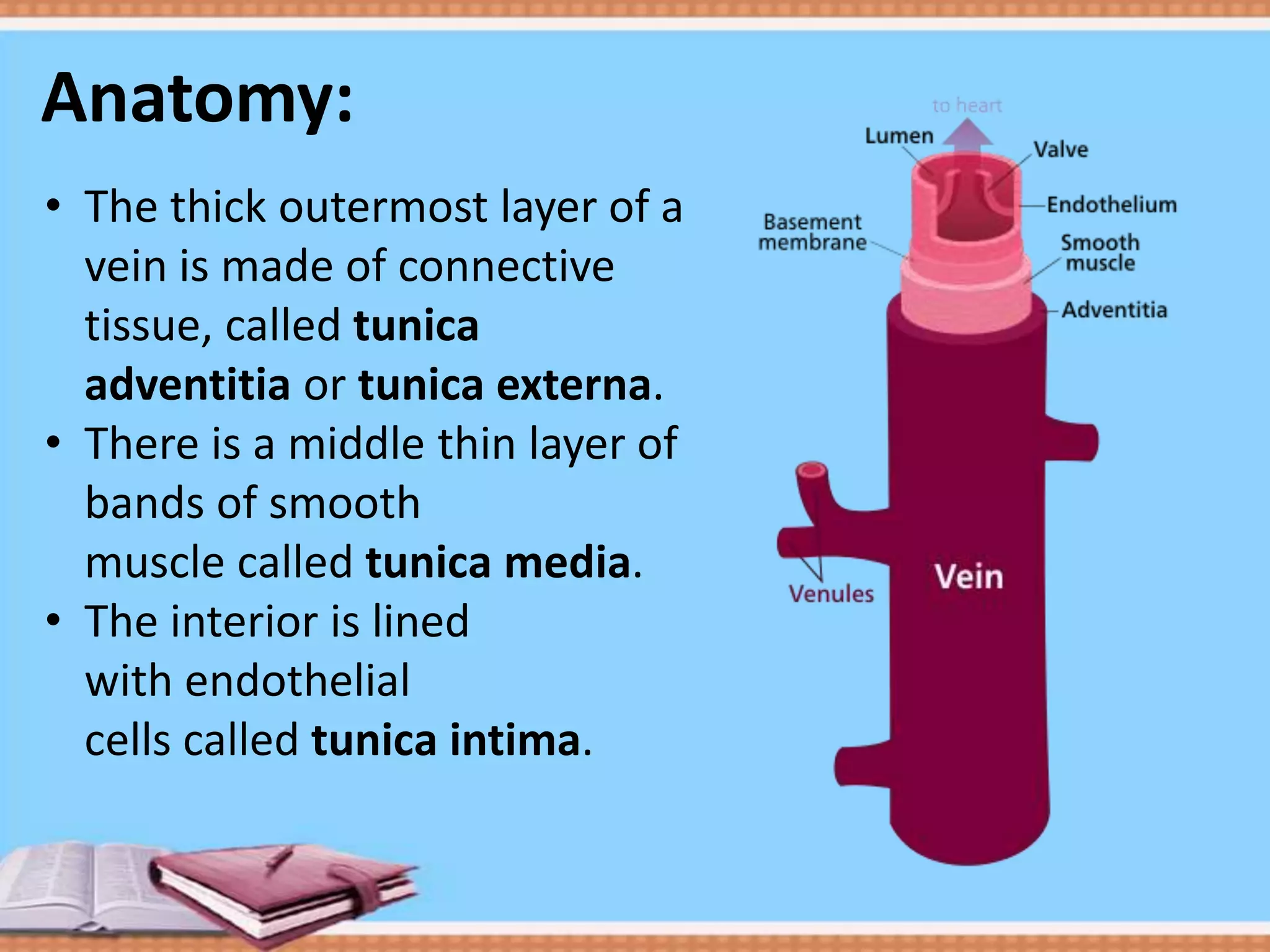
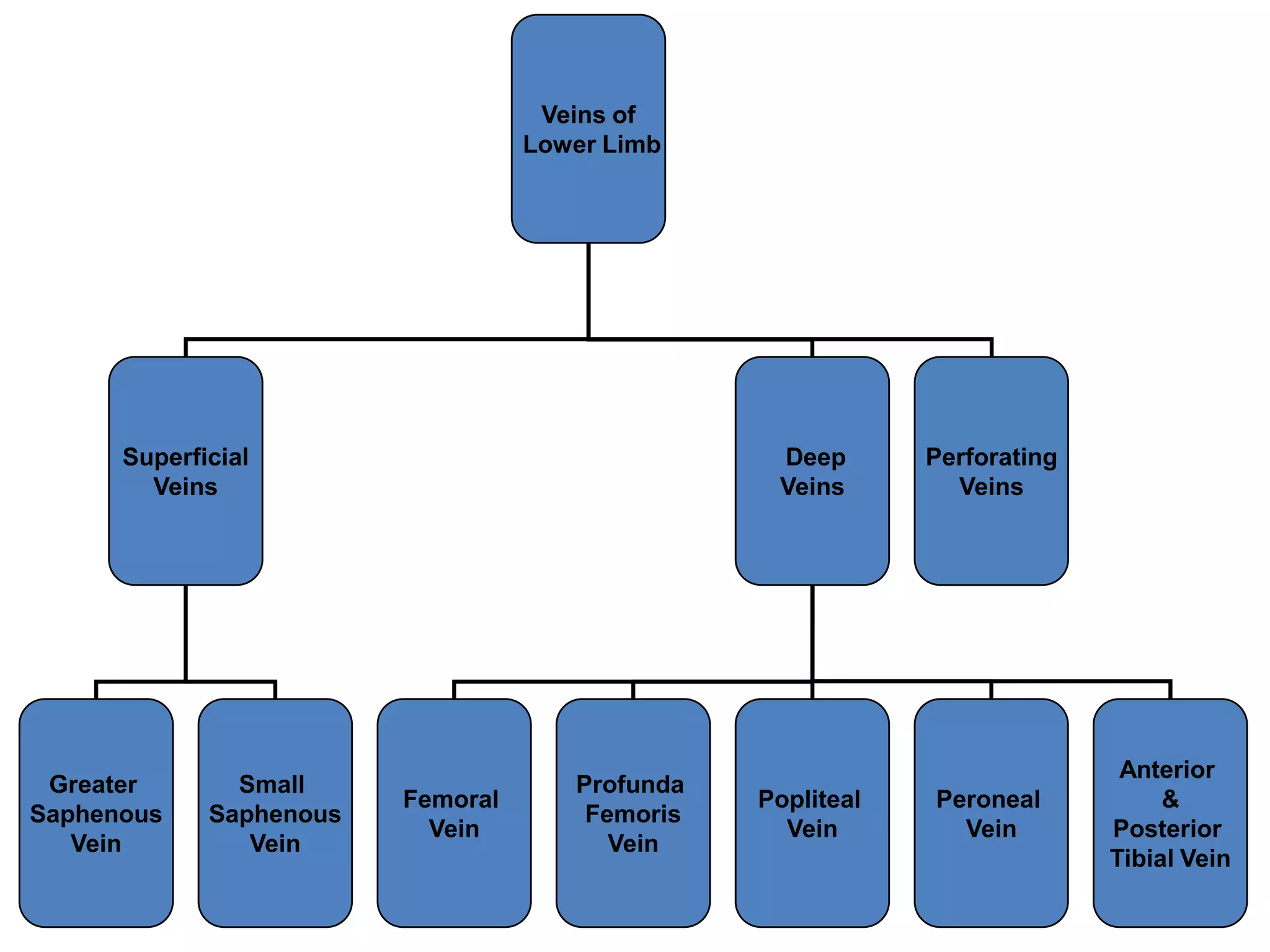
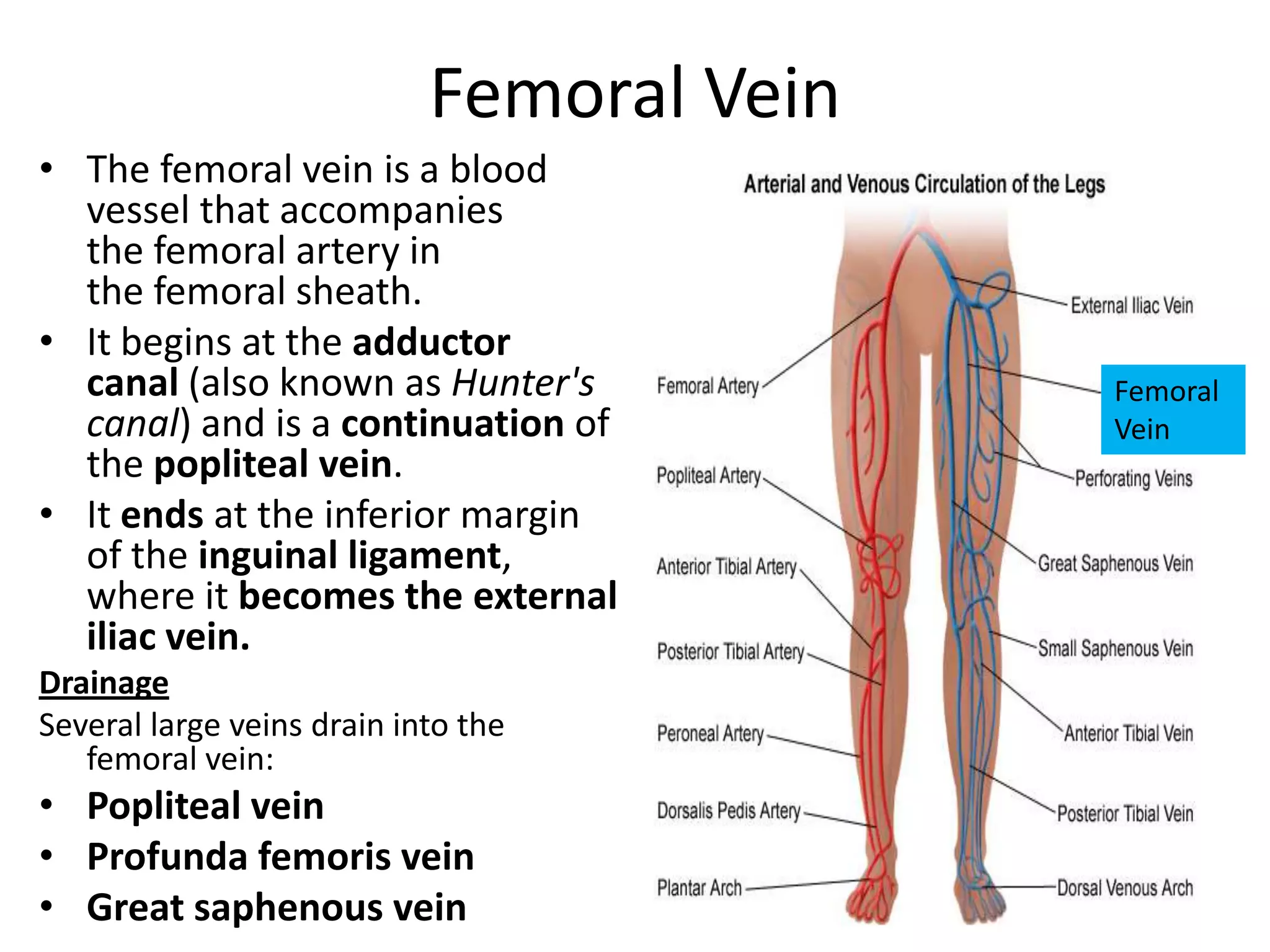
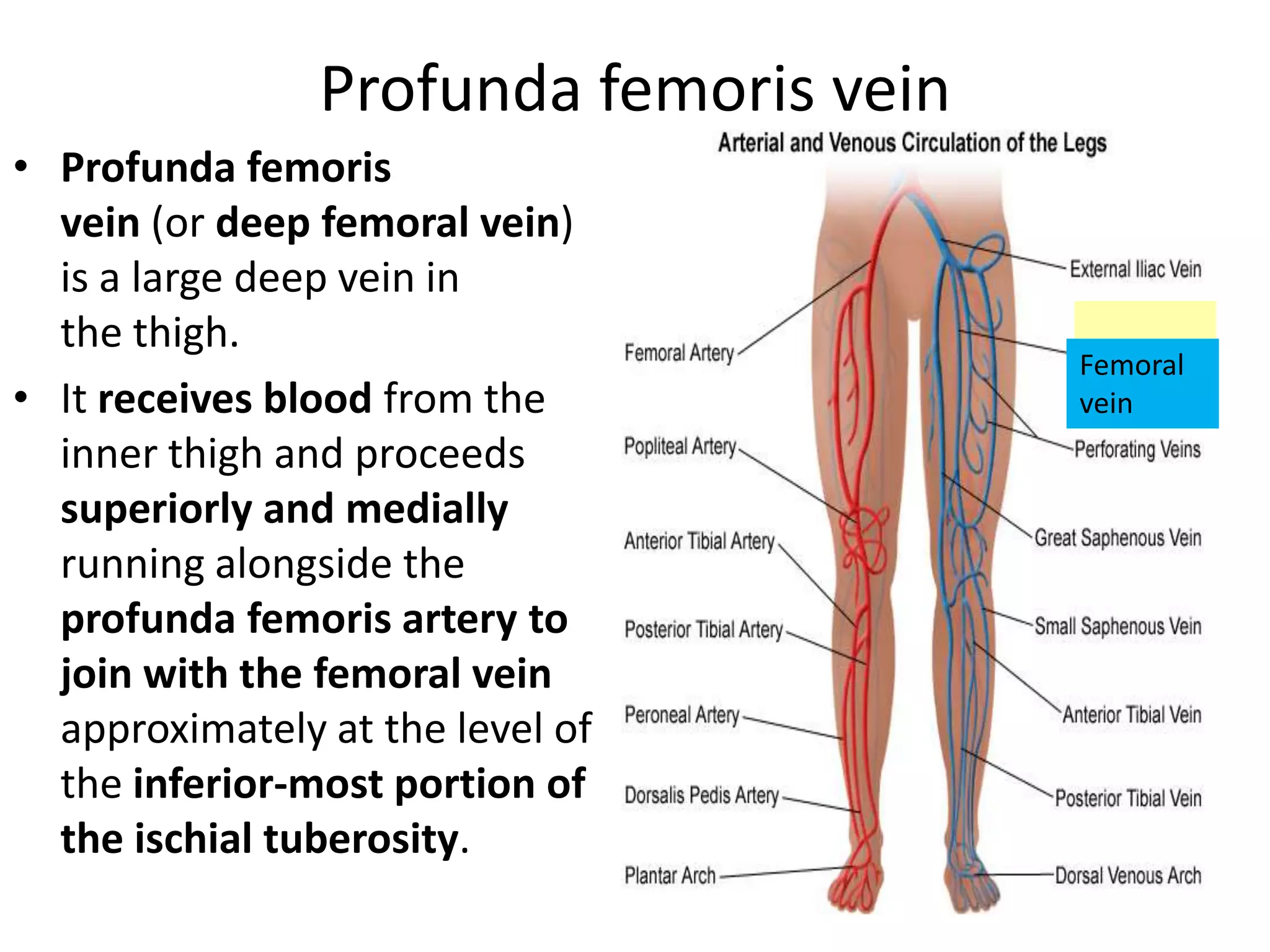
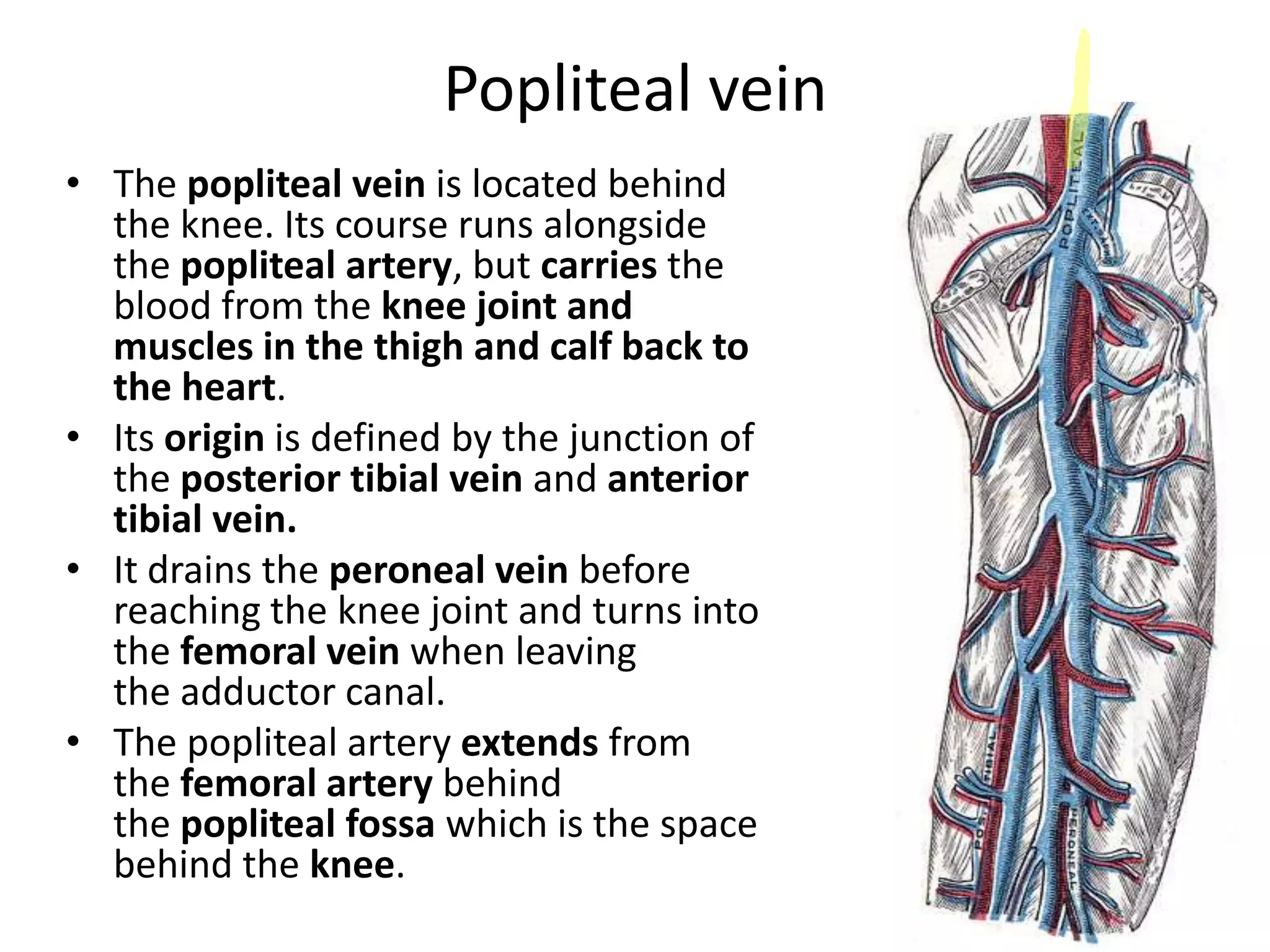
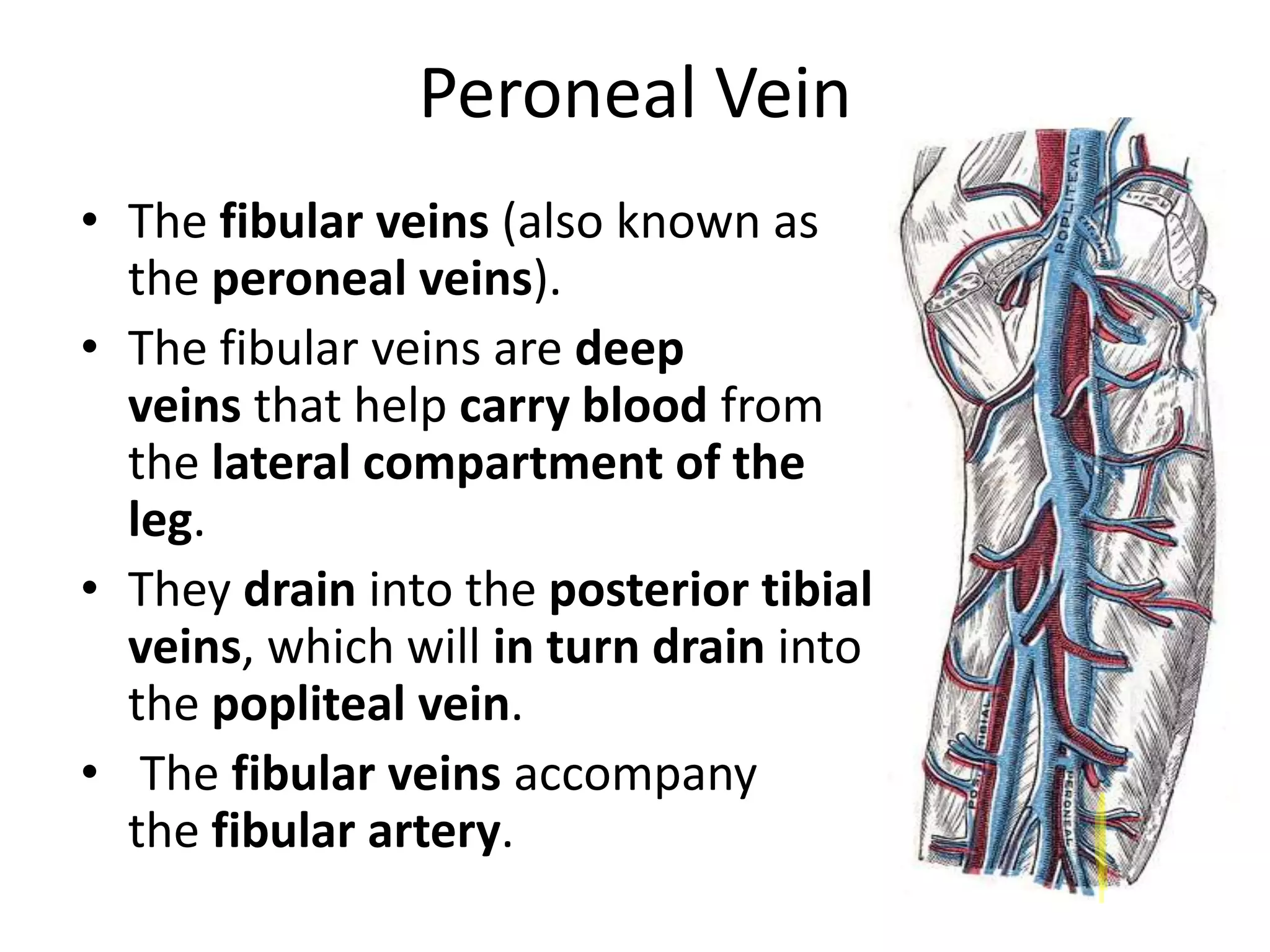
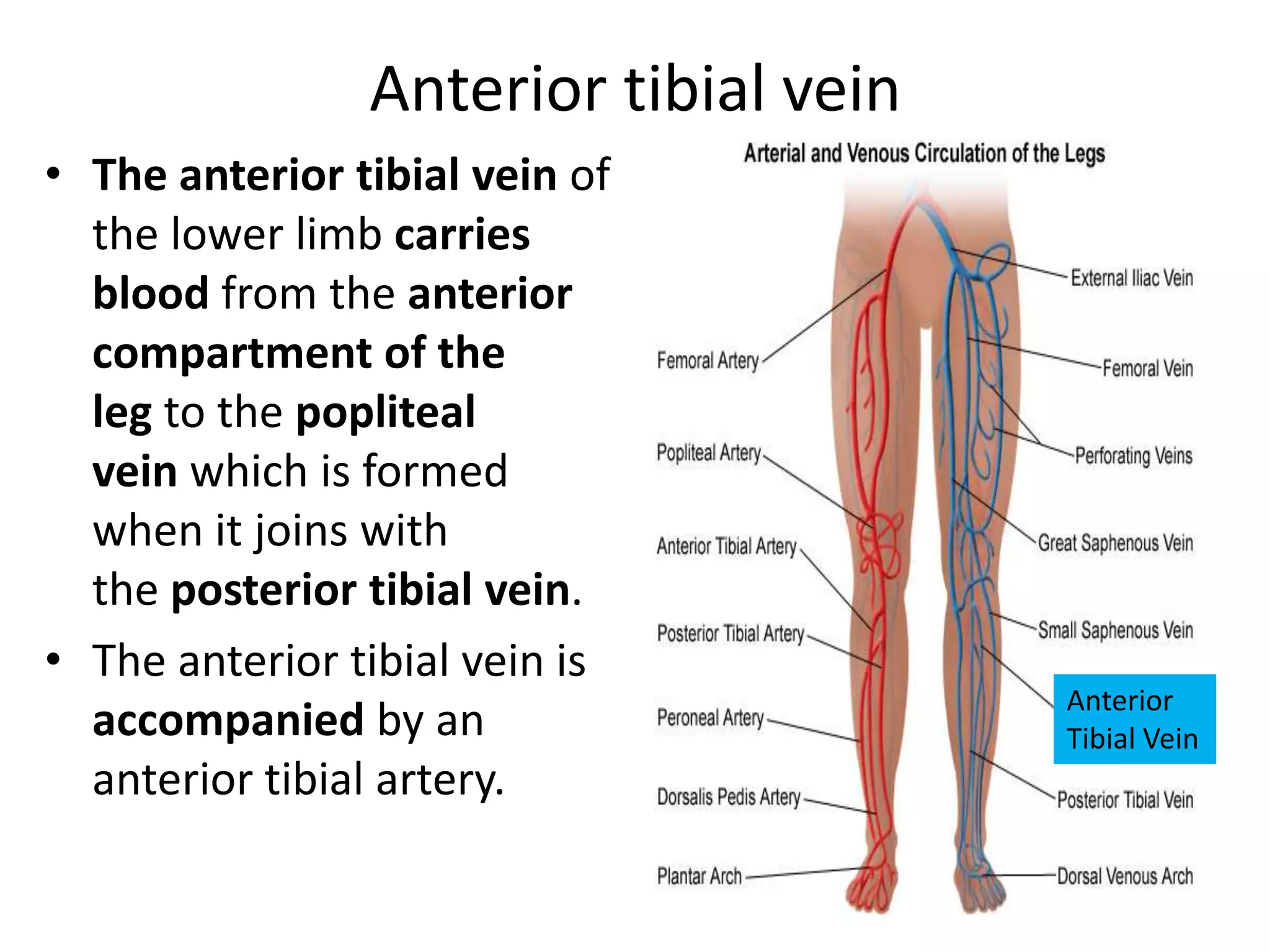
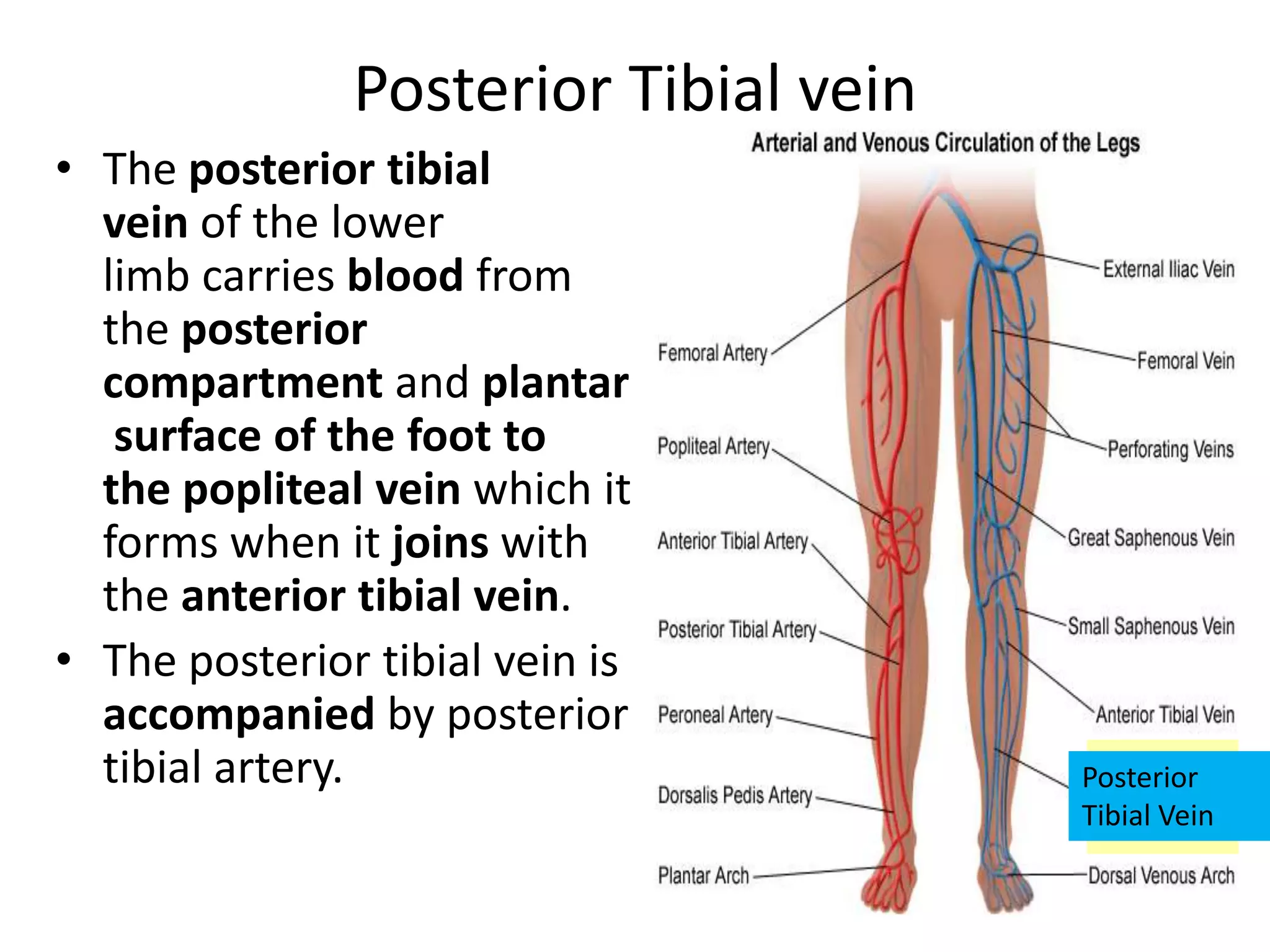
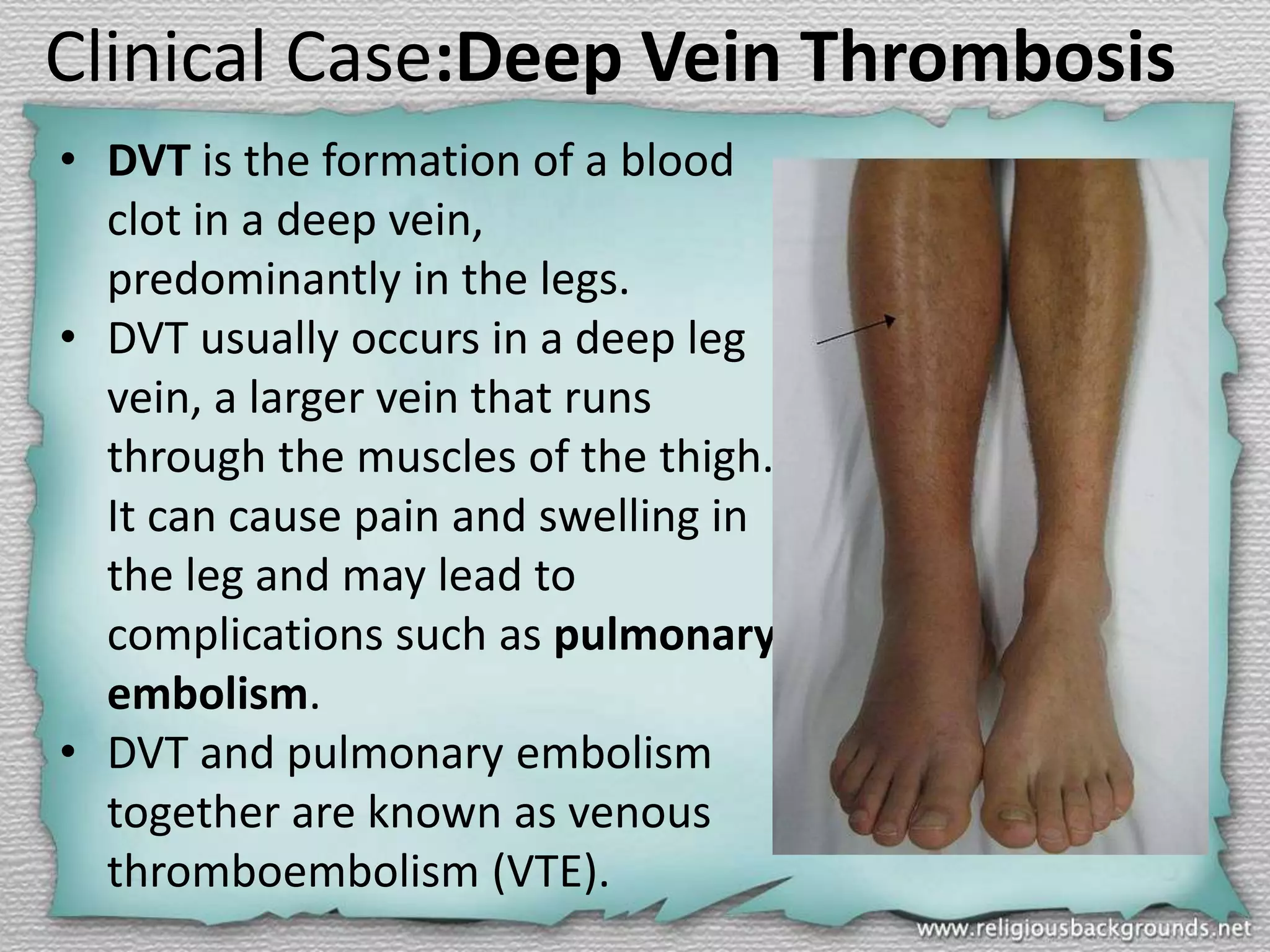
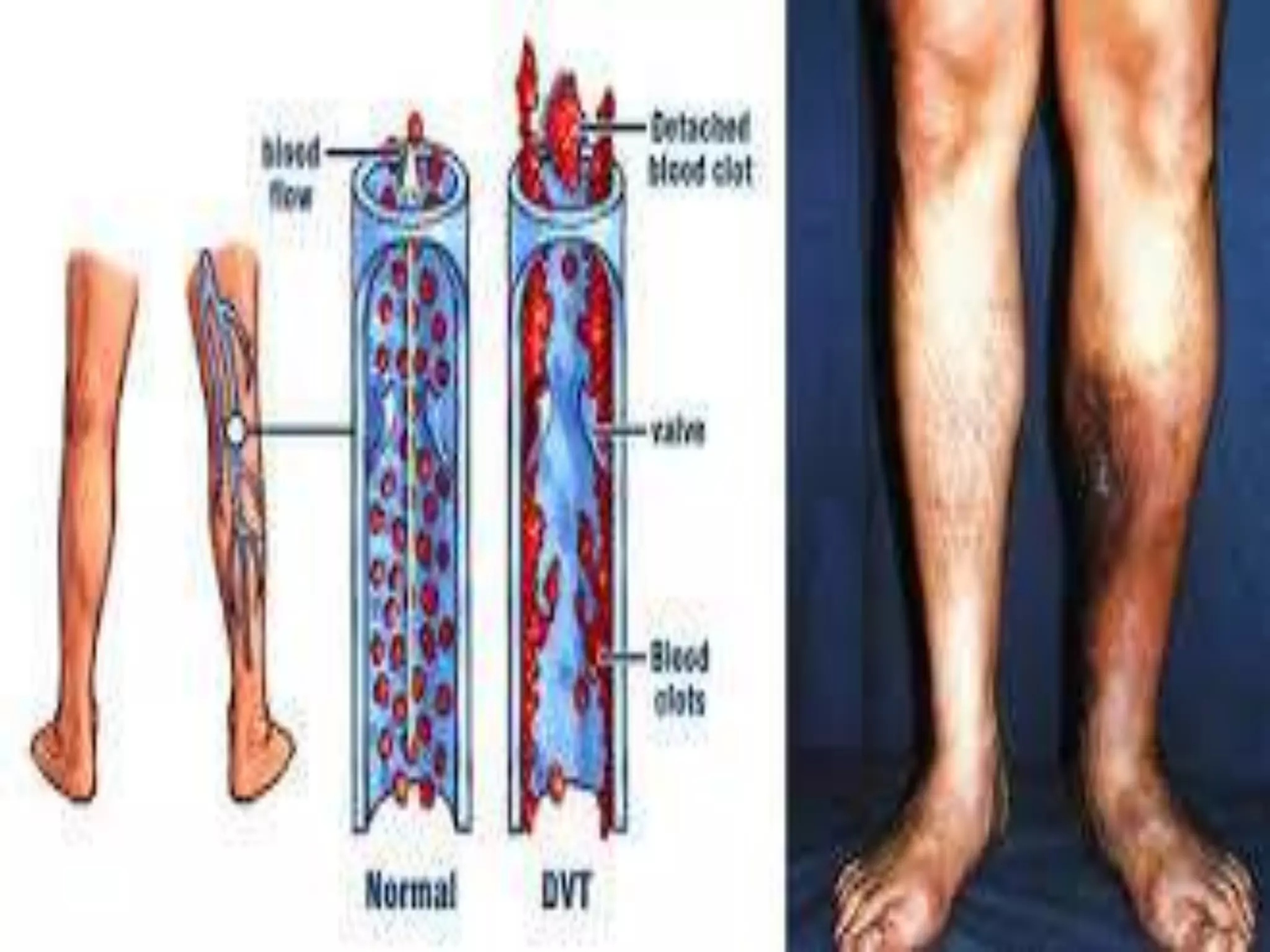
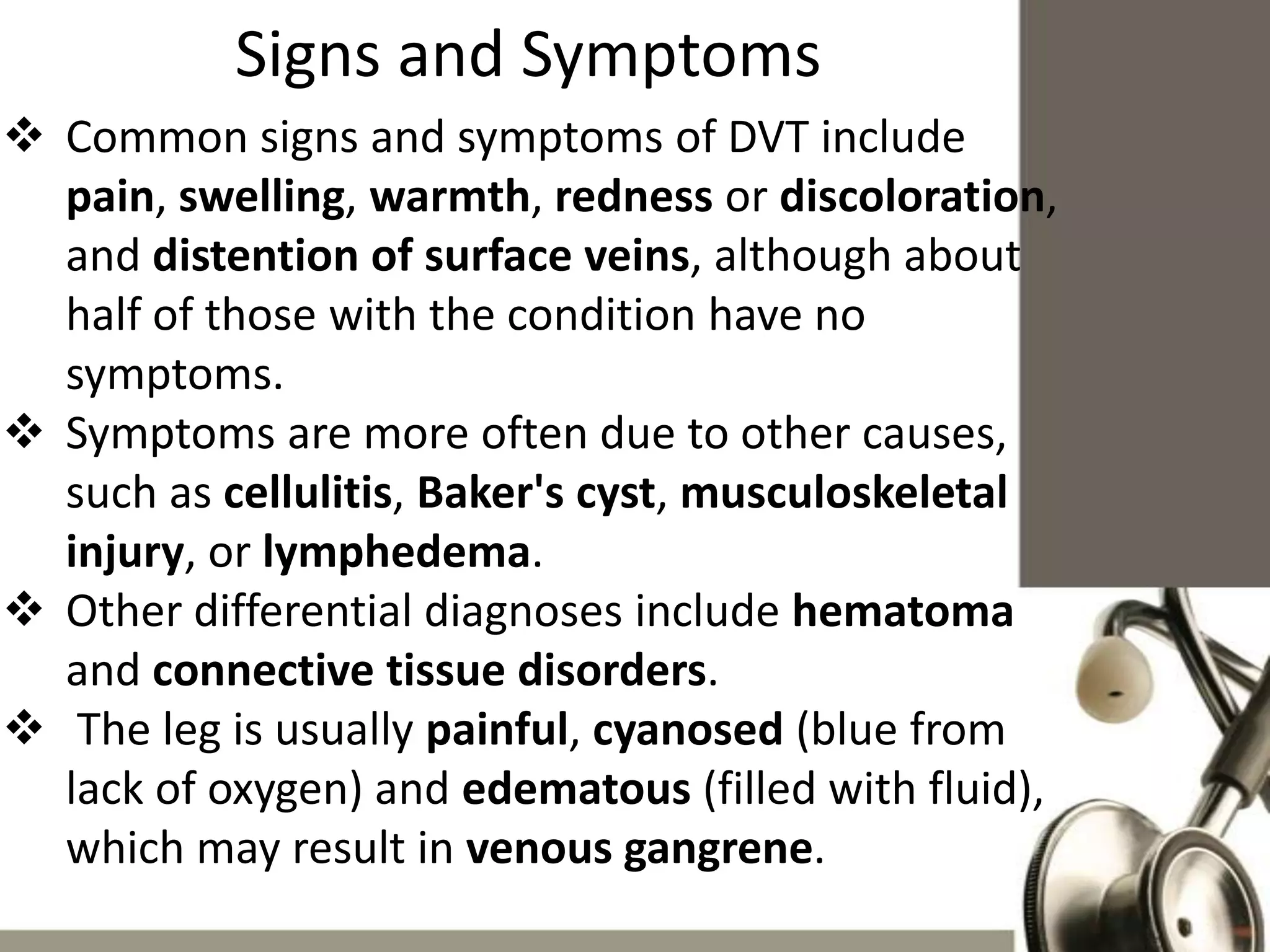
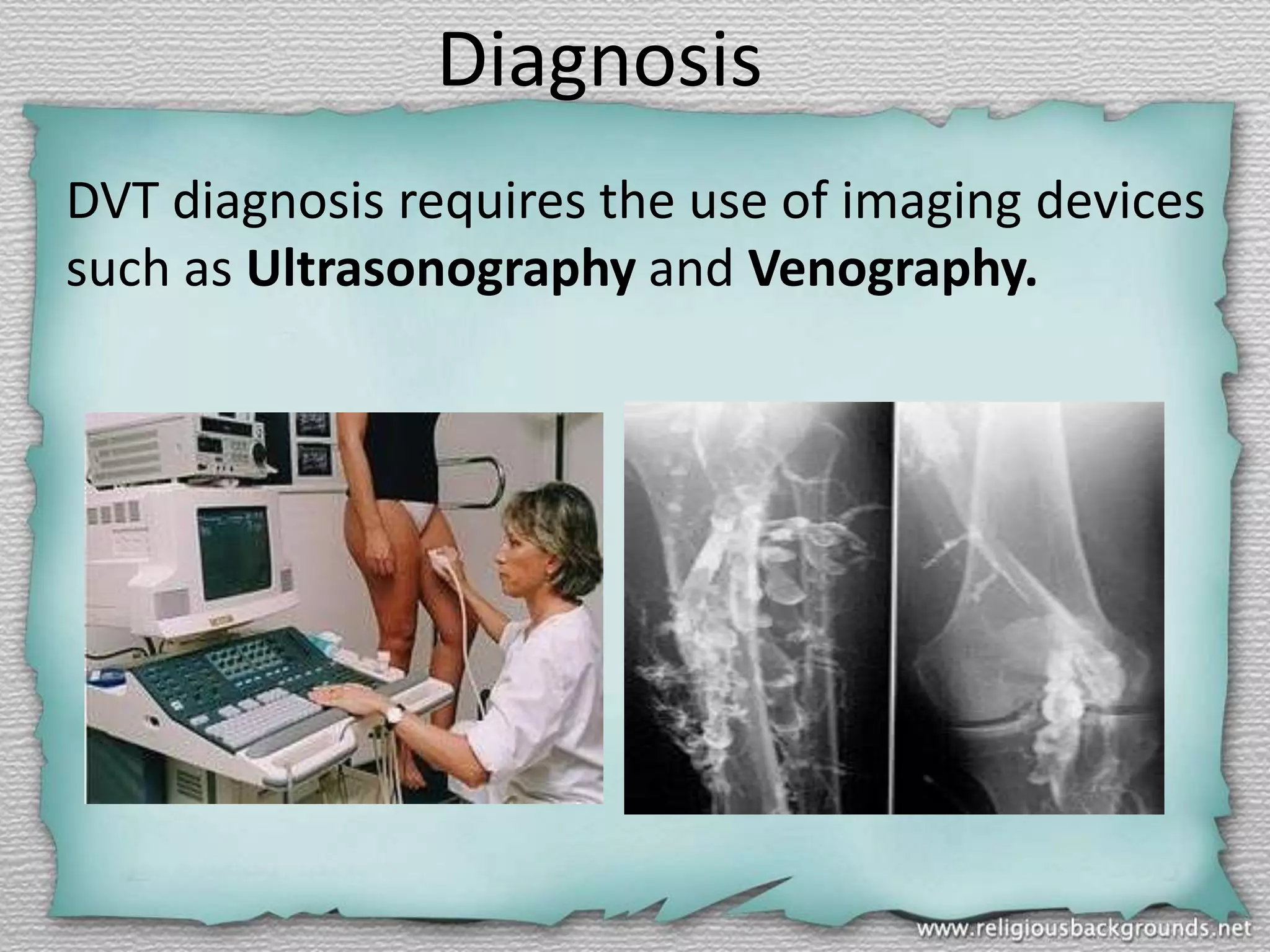
This document discusses the veins of the lower limb. It begins by describing the anatomy and classifications of veins in general. It then focuses on the specific veins of the lower limb, including the superficial greater and small saphenous veins and deep femoral, profunda femoris, popliteal, peroneal, anterior tibial, and posterior tibial veins. The document concludes by discussing deep vein thrombosis (DVT), its causes, symptoms, diagnosis, and treatments including anticoagulation and compression stockings.