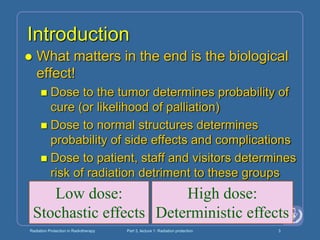
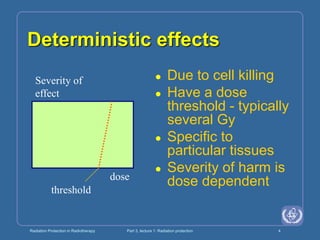
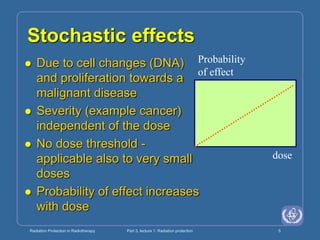
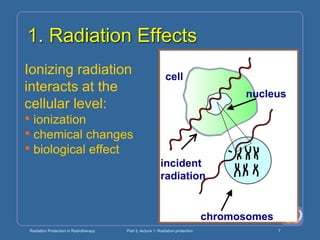
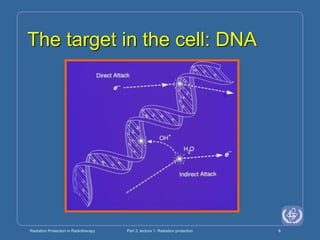
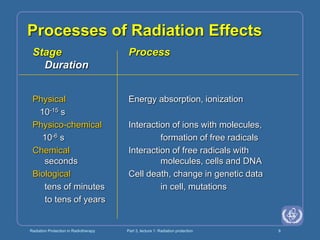
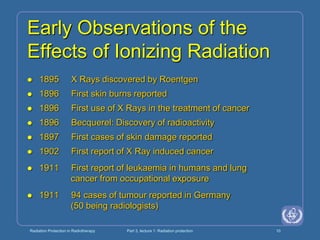
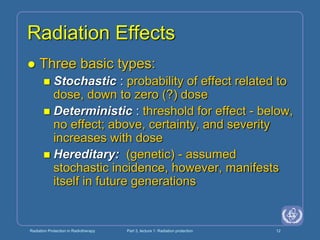
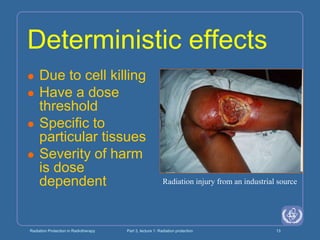
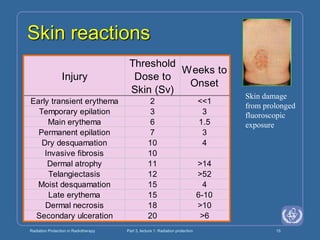
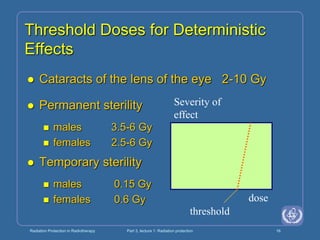
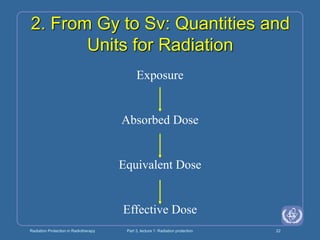
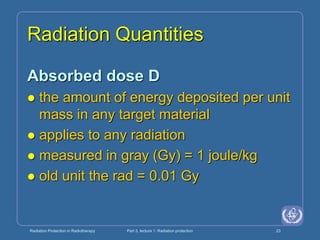
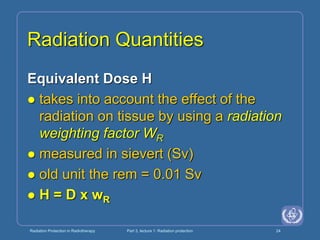
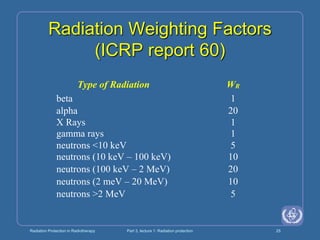
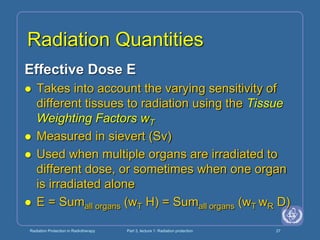
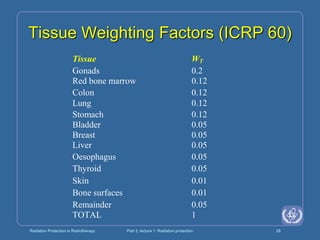
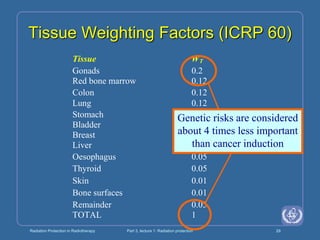
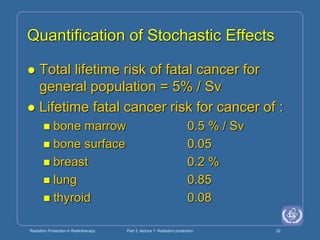
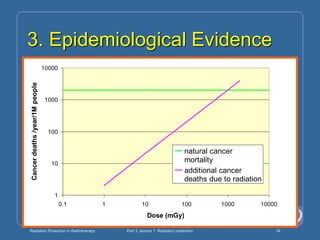
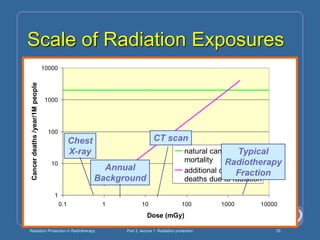
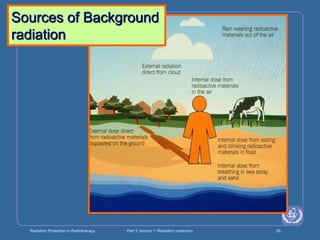
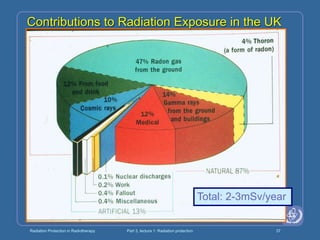
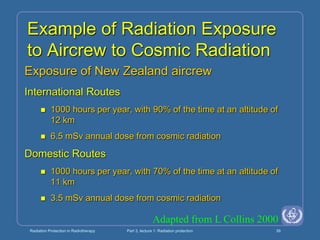
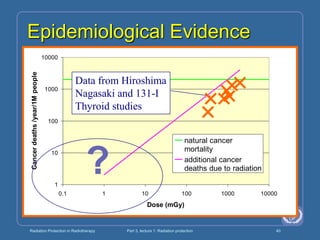
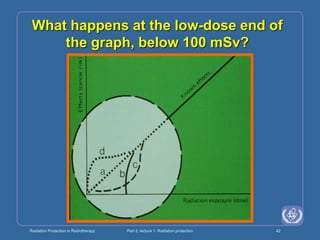
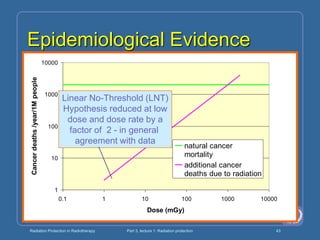
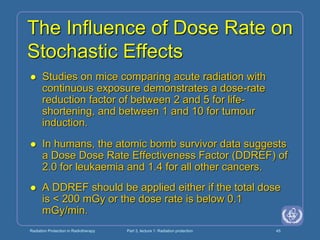
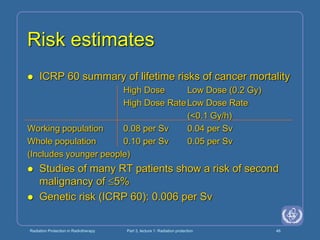
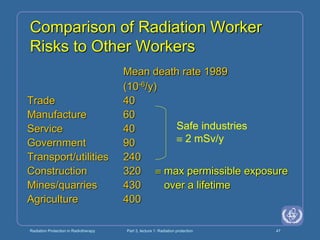
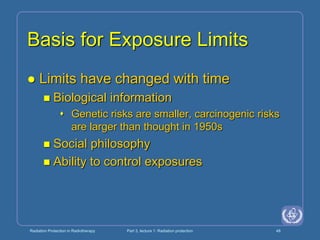
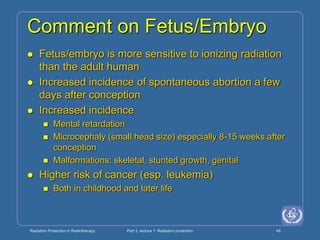
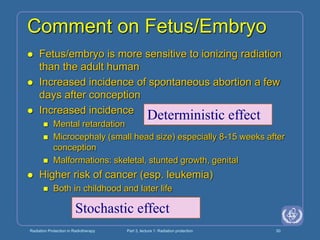
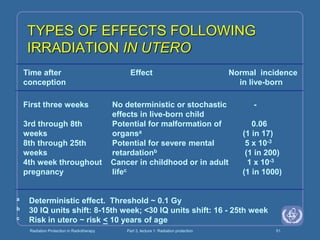
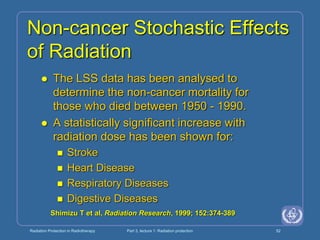
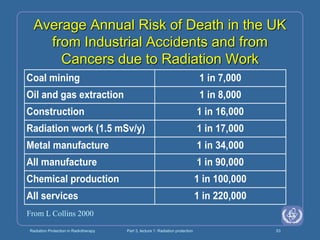
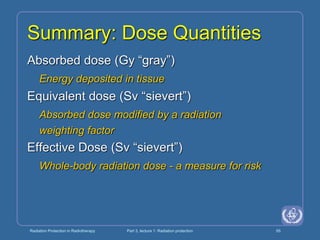
The document discusses the biological effects of ionizing radiation in the context of radiotherapy, highlighting the importance of radiation protection for patients, staff, and visitors. It delineates between deterministic effects, which exhibit a dose threshold, and stochastic effects, which occur probabilistically without a threshold. Additionally, the text covers radiation quantities, risk assessment, and epidemiological evidence related to cancer induction from radiation exposure.