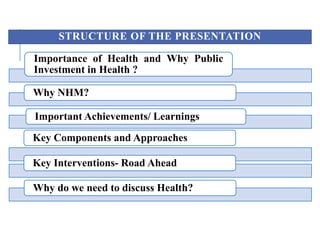
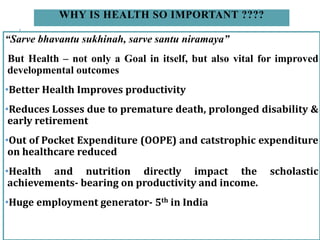
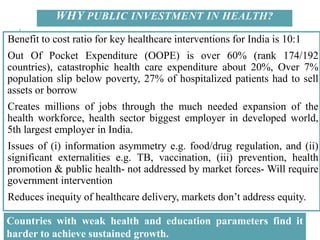
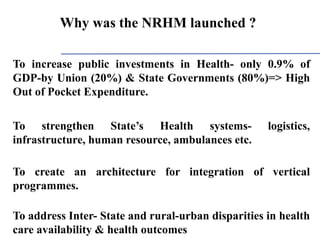
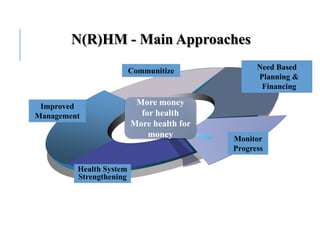
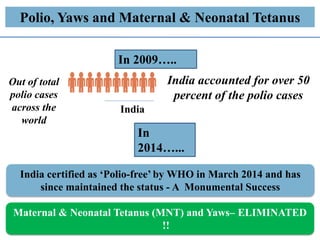
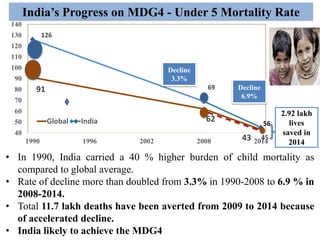
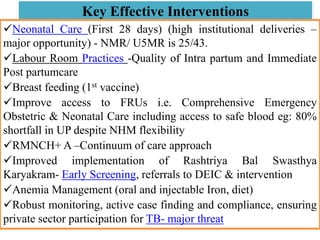
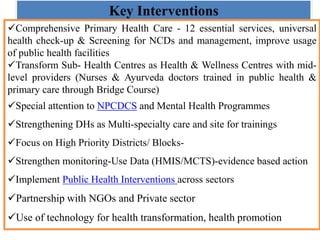
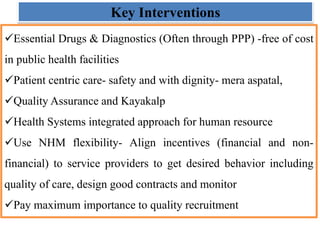
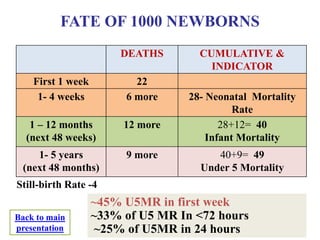
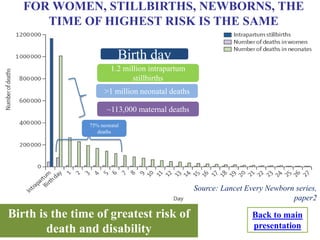
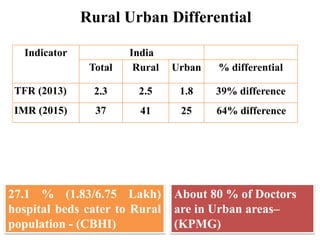
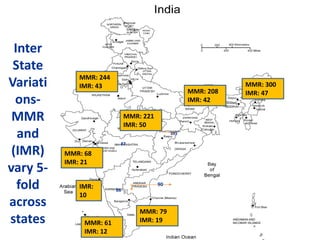
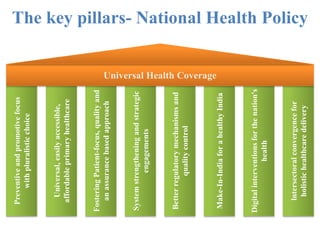
This document provides an overview of the key elements, achievements, and challenges of the National Health Mission (NHM) in India. It discusses how NHM has strengthened India's public health system and led to important health improvements, but that challenges remain. Key interventions and priorities for the road ahead are also outlined.