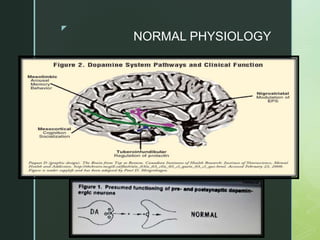
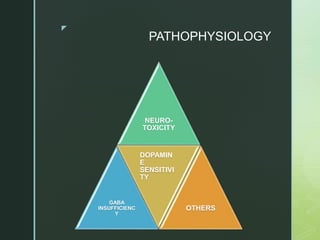
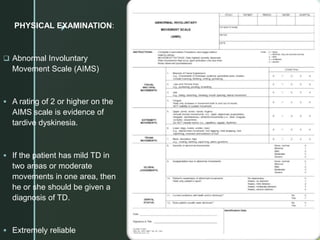
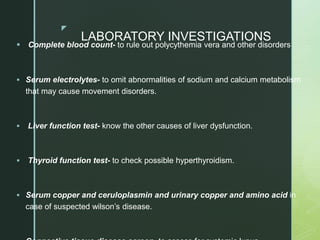
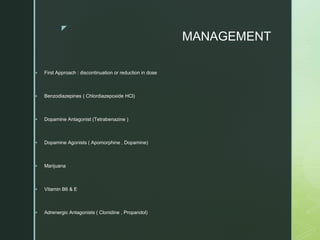
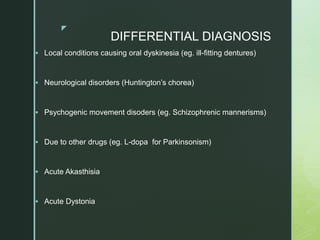
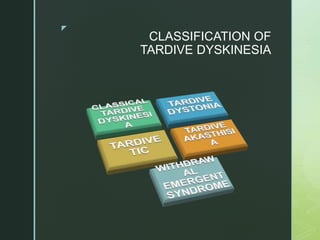
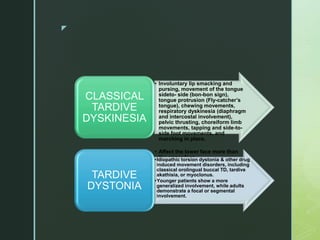
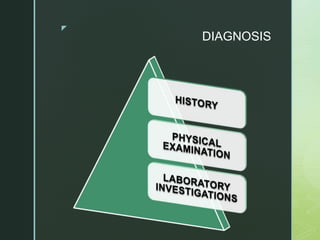
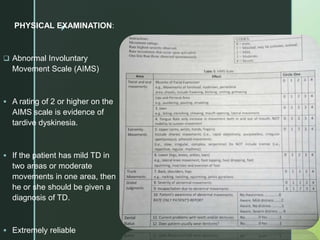
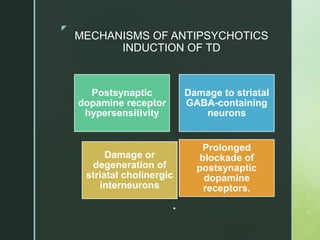
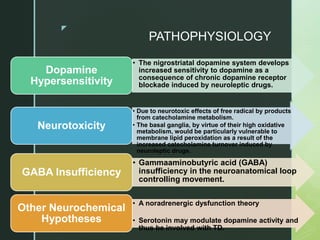
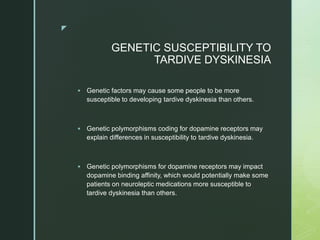
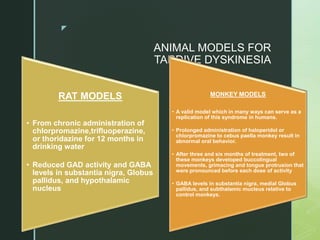
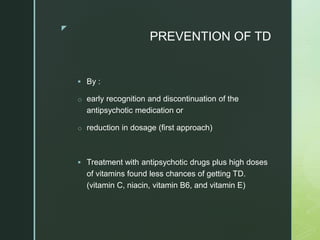
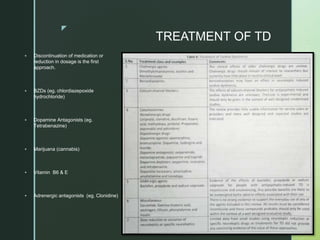
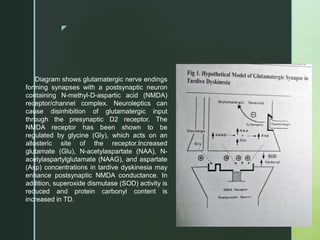
This document provides an overview of orofacial dyskinesia, also known as tardive dyskinesia. It begins with an introduction defining orofacial dyskinesia as involuntary, repetitive stereotyped movements involving the head, face, and oral structures. It then discusses the etiology, typically being drug-induced by antipsychotics, and risk factors like older age, female sex, and long-term antipsychotic use. The document outlines the clinical features, diagnosis using scales like AIMS, management beginning with discontinuing the offending drug, and differential diagnosis from other movement disorders.
![z
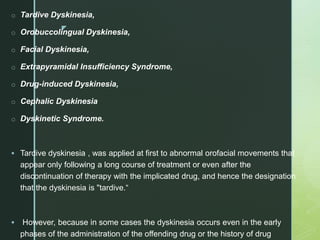
ETIOLOGY
Drug-induced [most common]
( anti-psychotics like phenothiazines & butyrophenones ; anti-
Parkinsonian like L-dopa )
Other proposed etiological factors :
Brain damage
( leukotomies , ECT in chronic Schizophrenia)
Spontaneous (rare , 1-2 % )
Dental malocclusion / Edentulous state](https://image.slidesharecdn.com/jcorofacialdyskinesia-220927091305-443b9256/85/JC-OROFACIAL-DYSKINESIA-pptx-4-320.jpg)