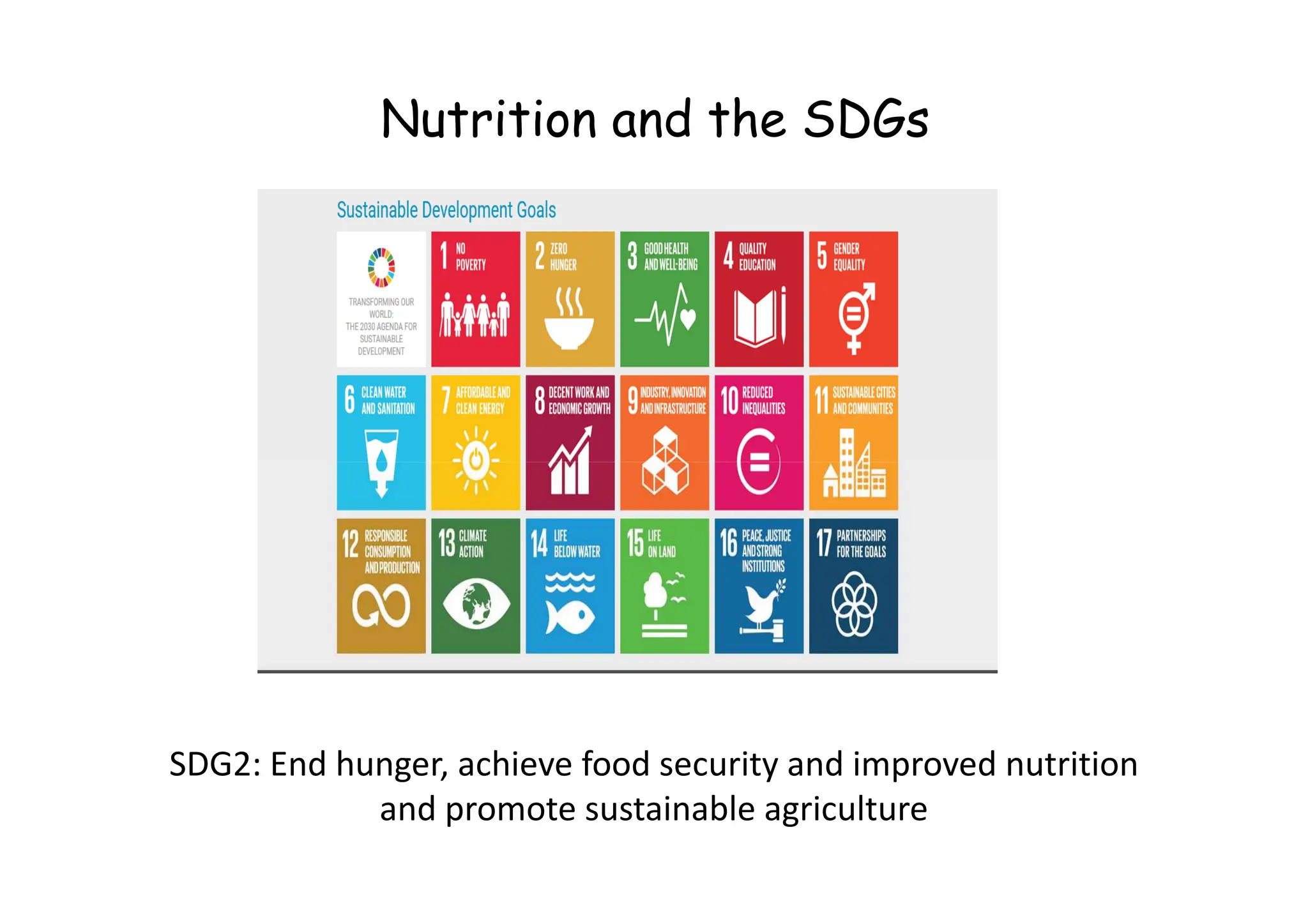
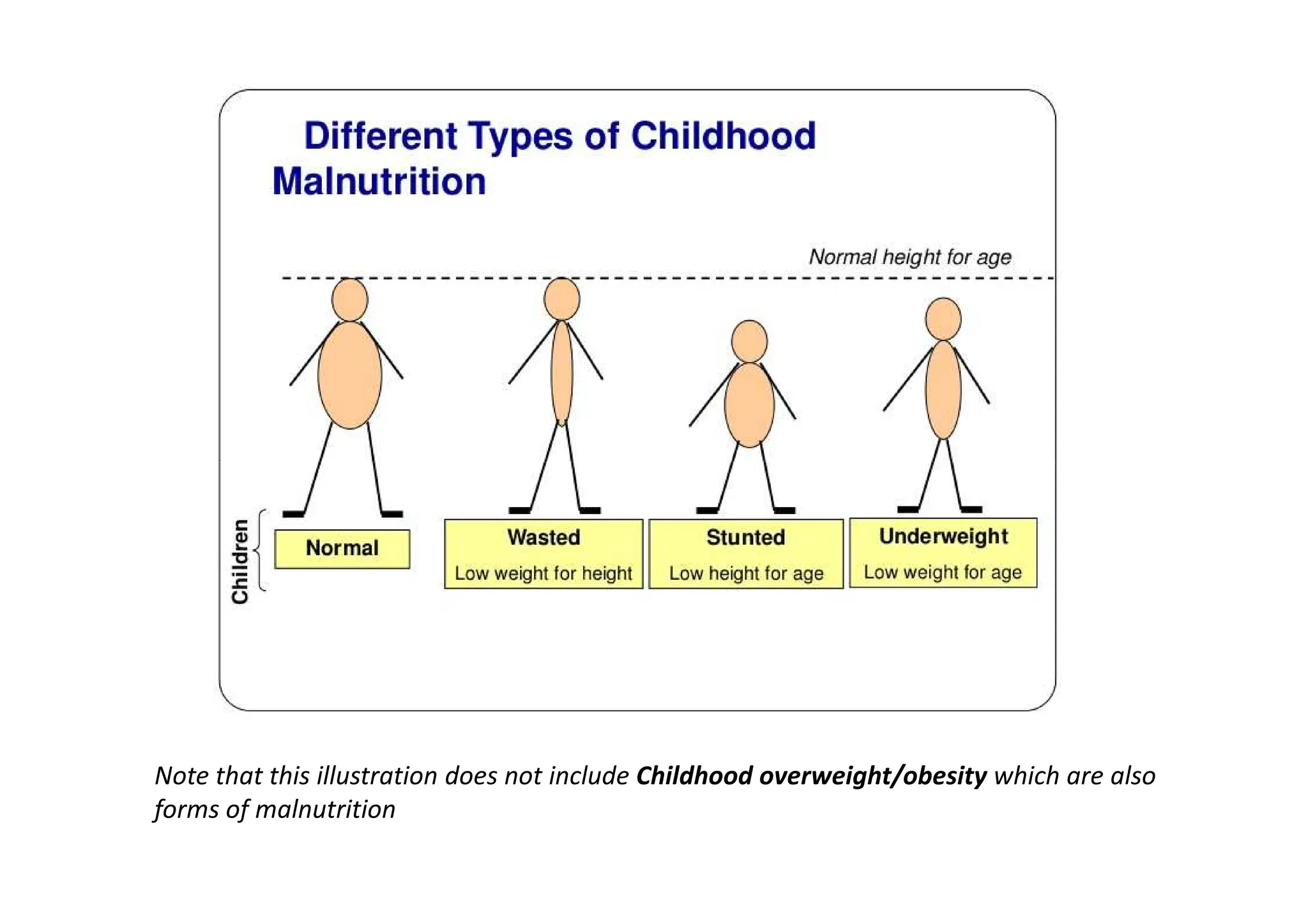
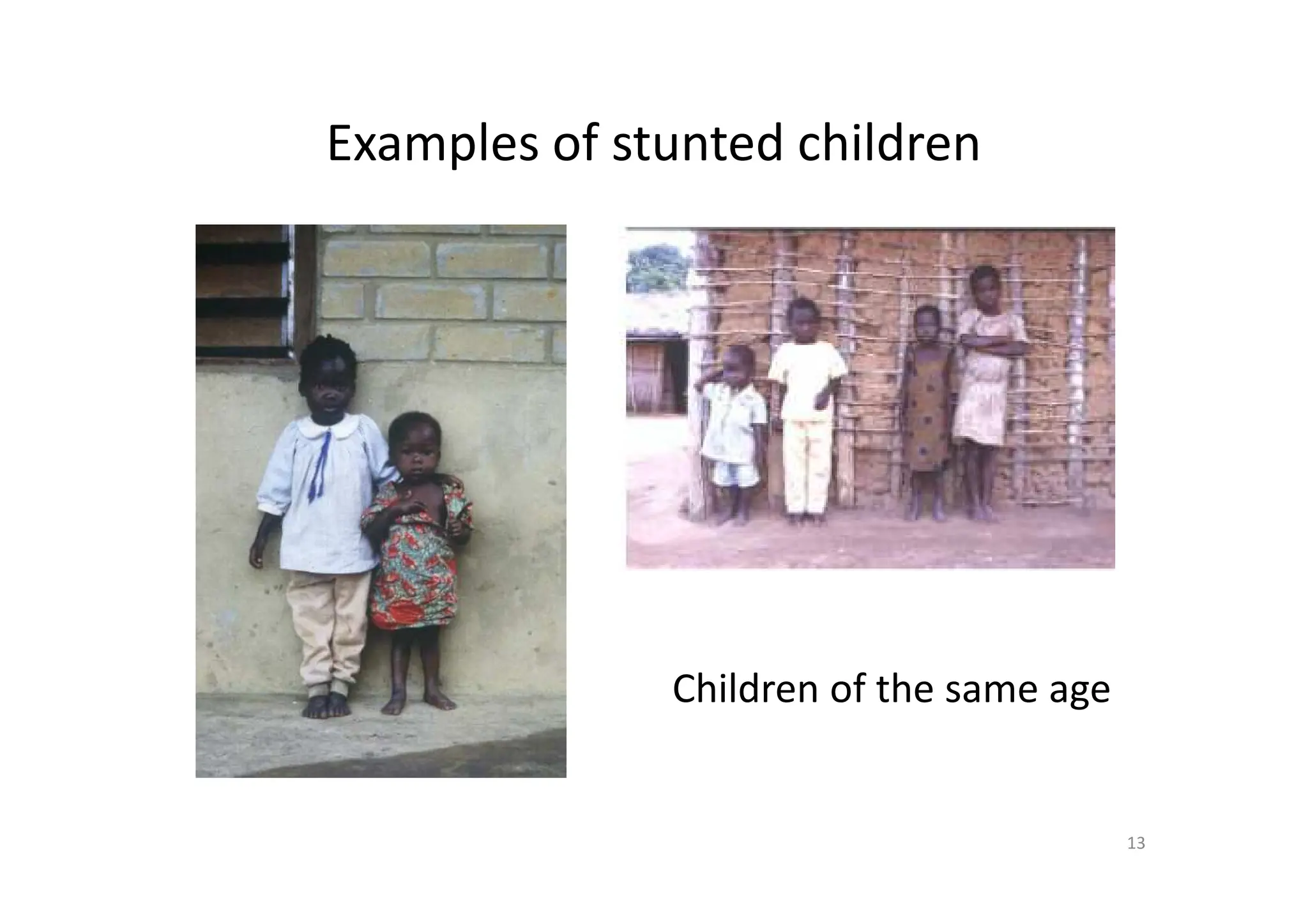
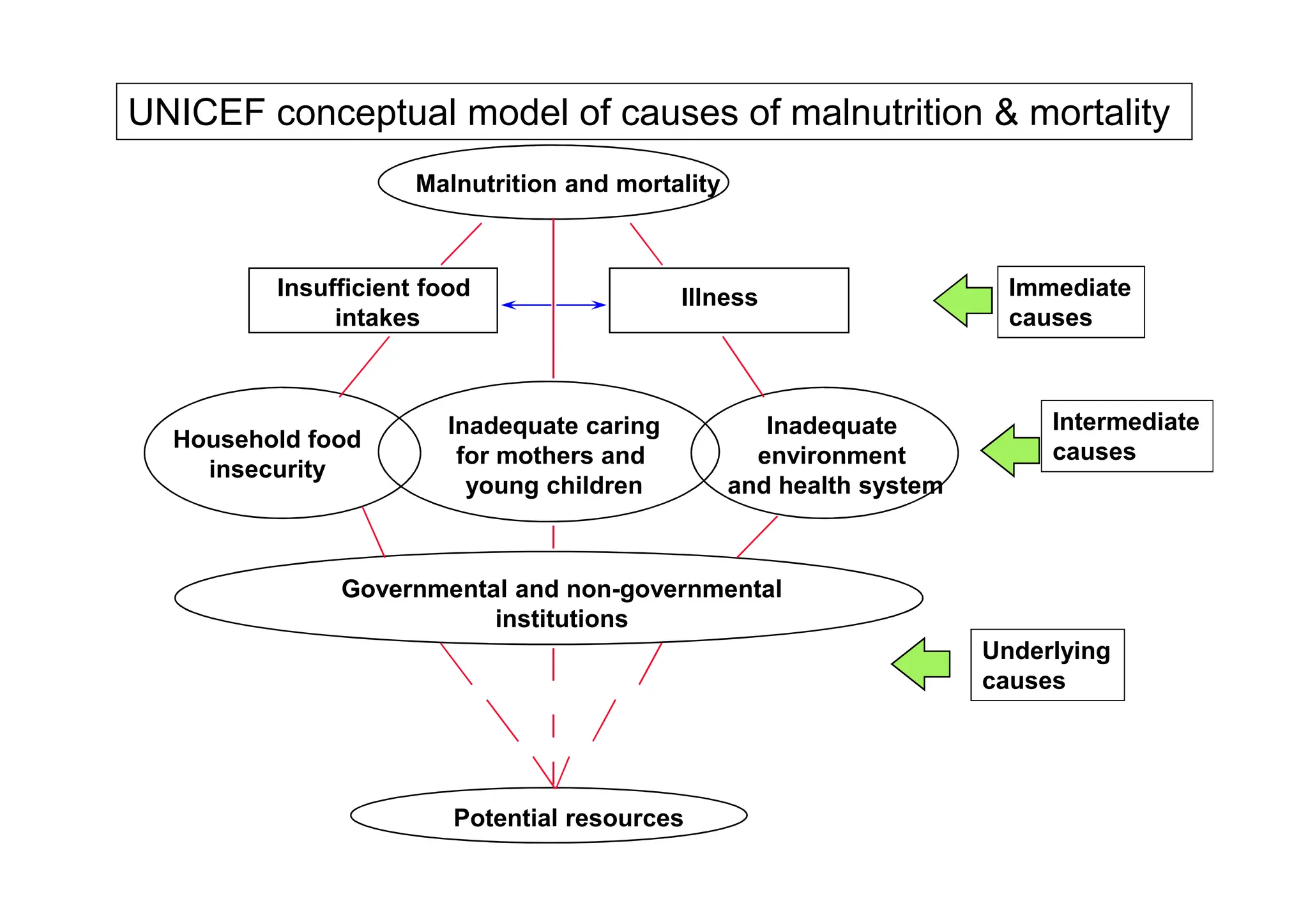
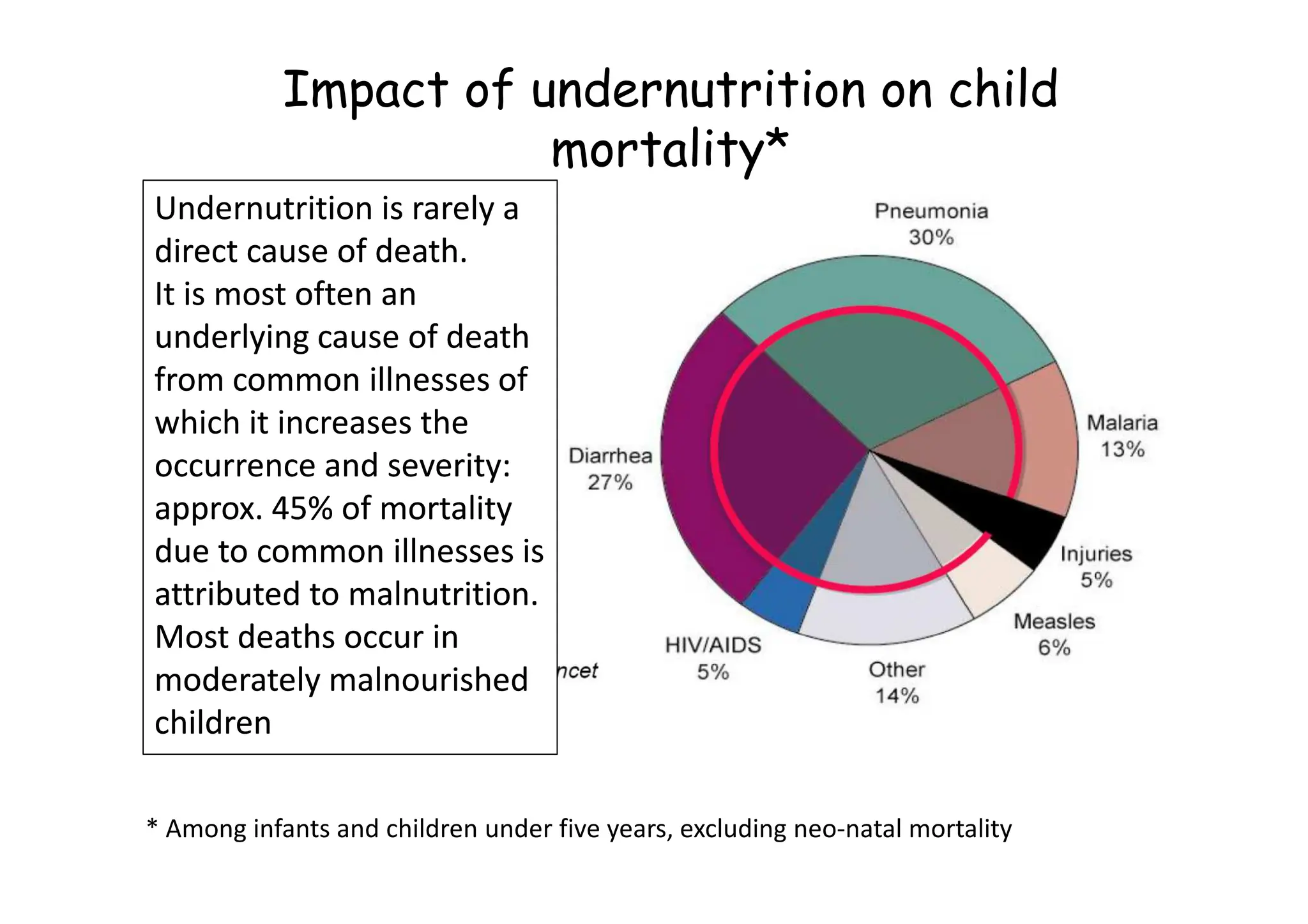
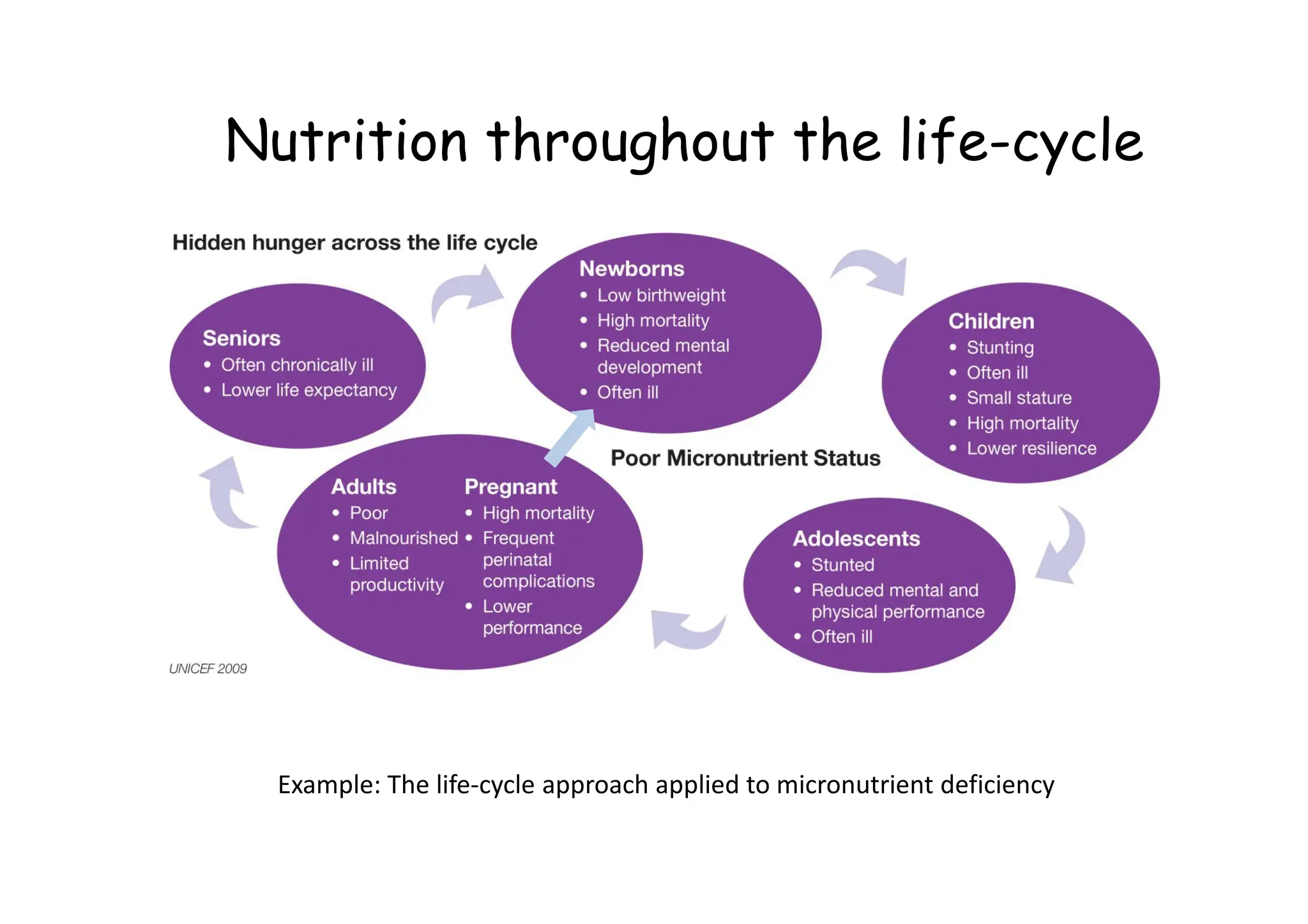
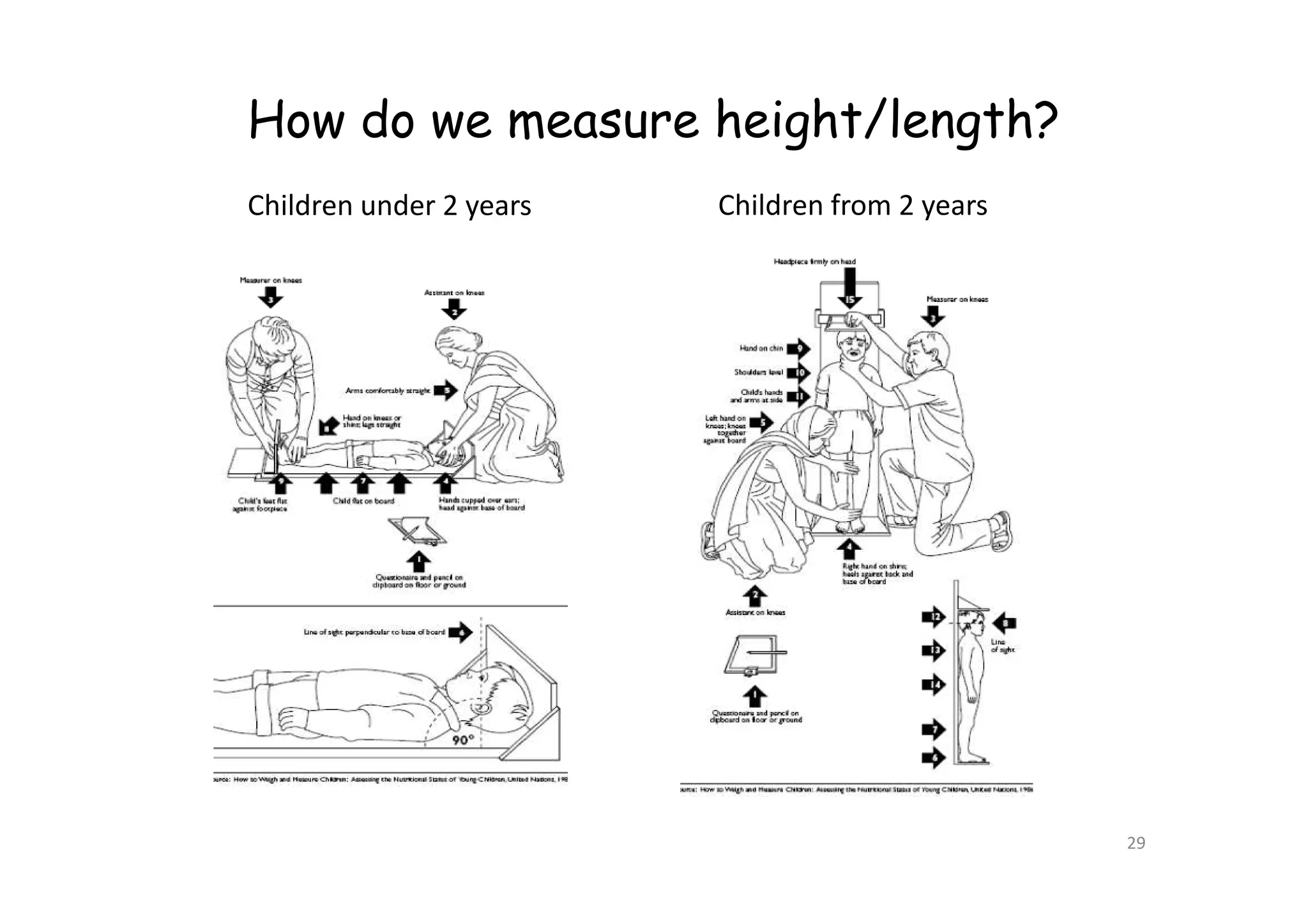
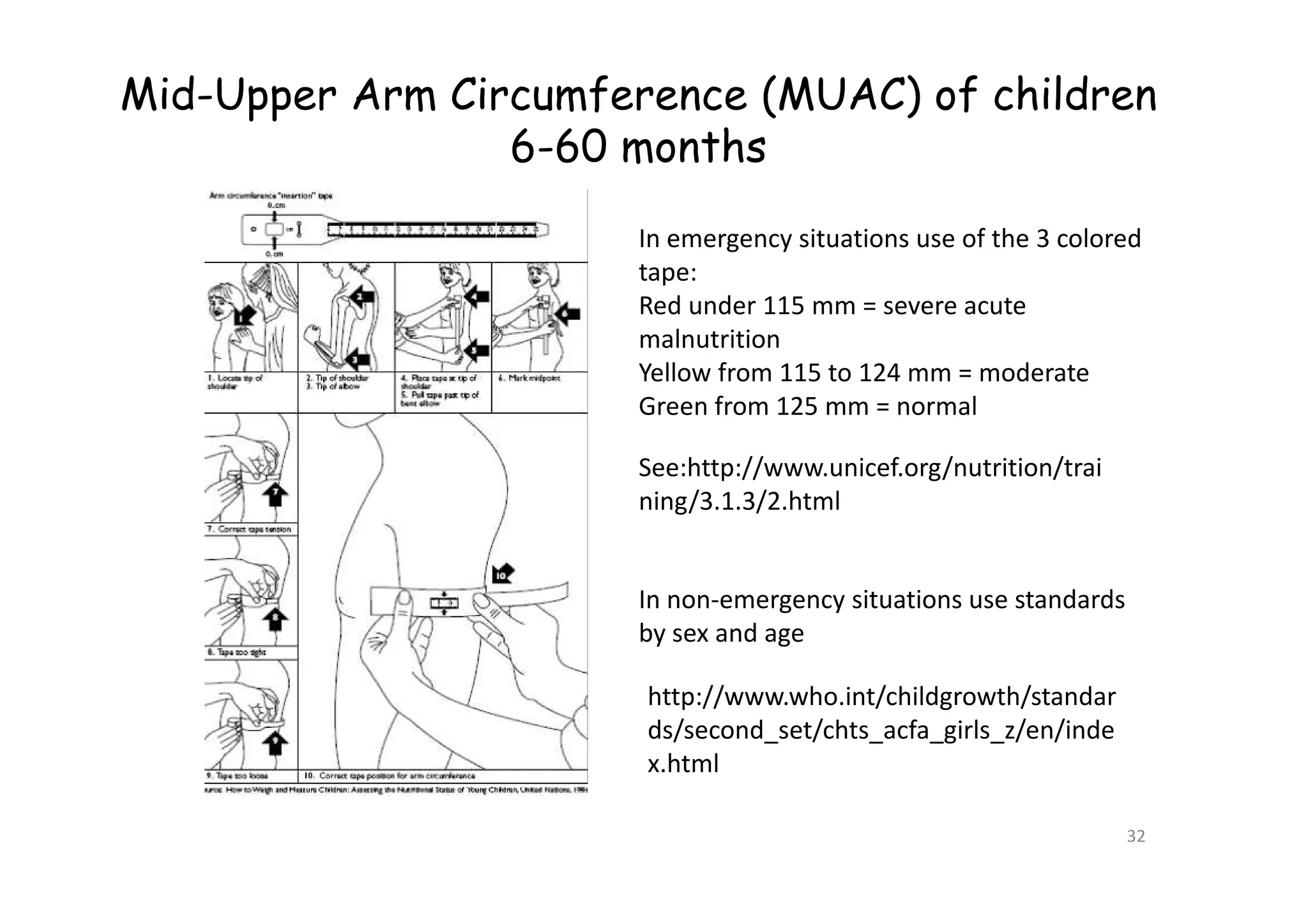
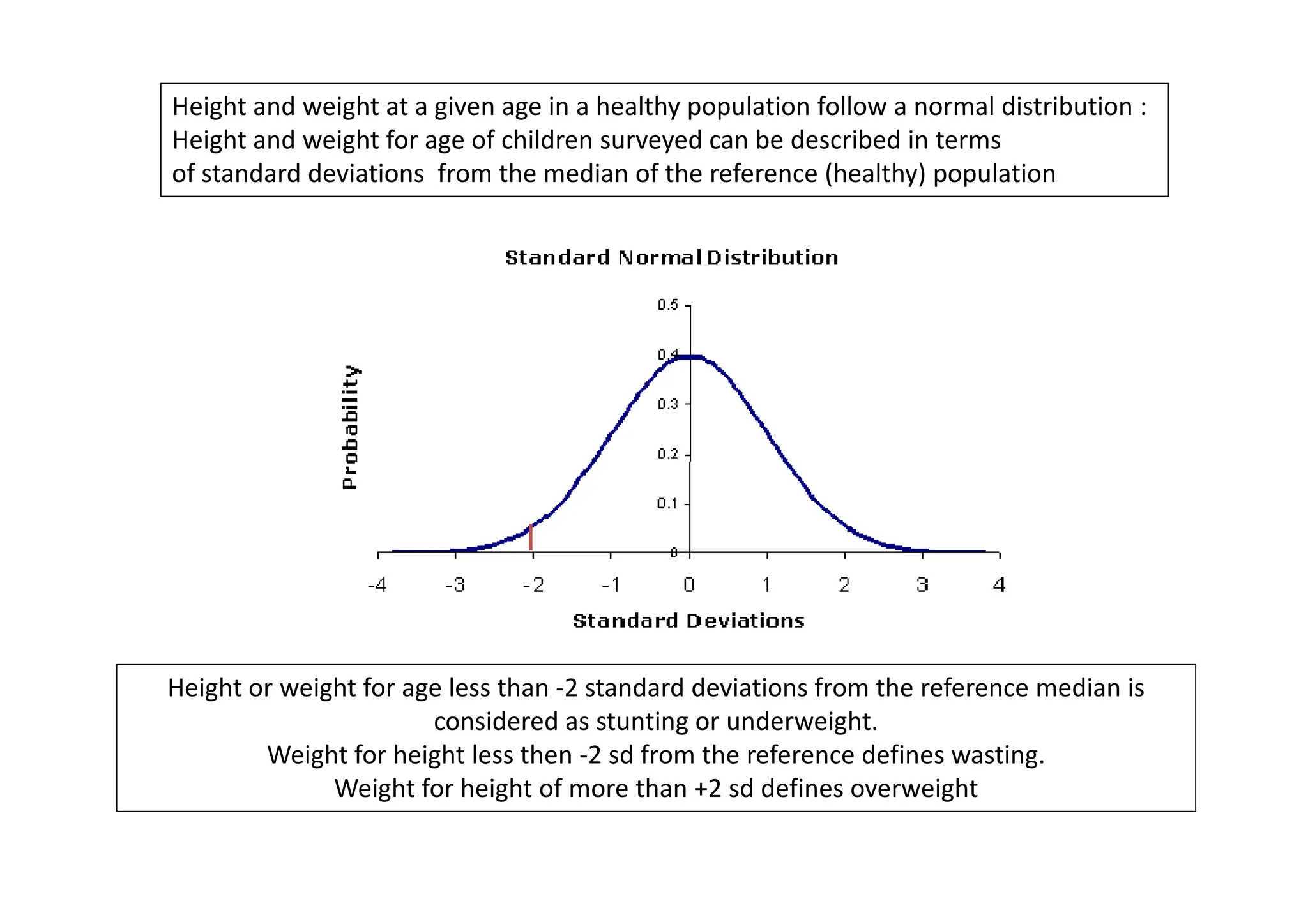
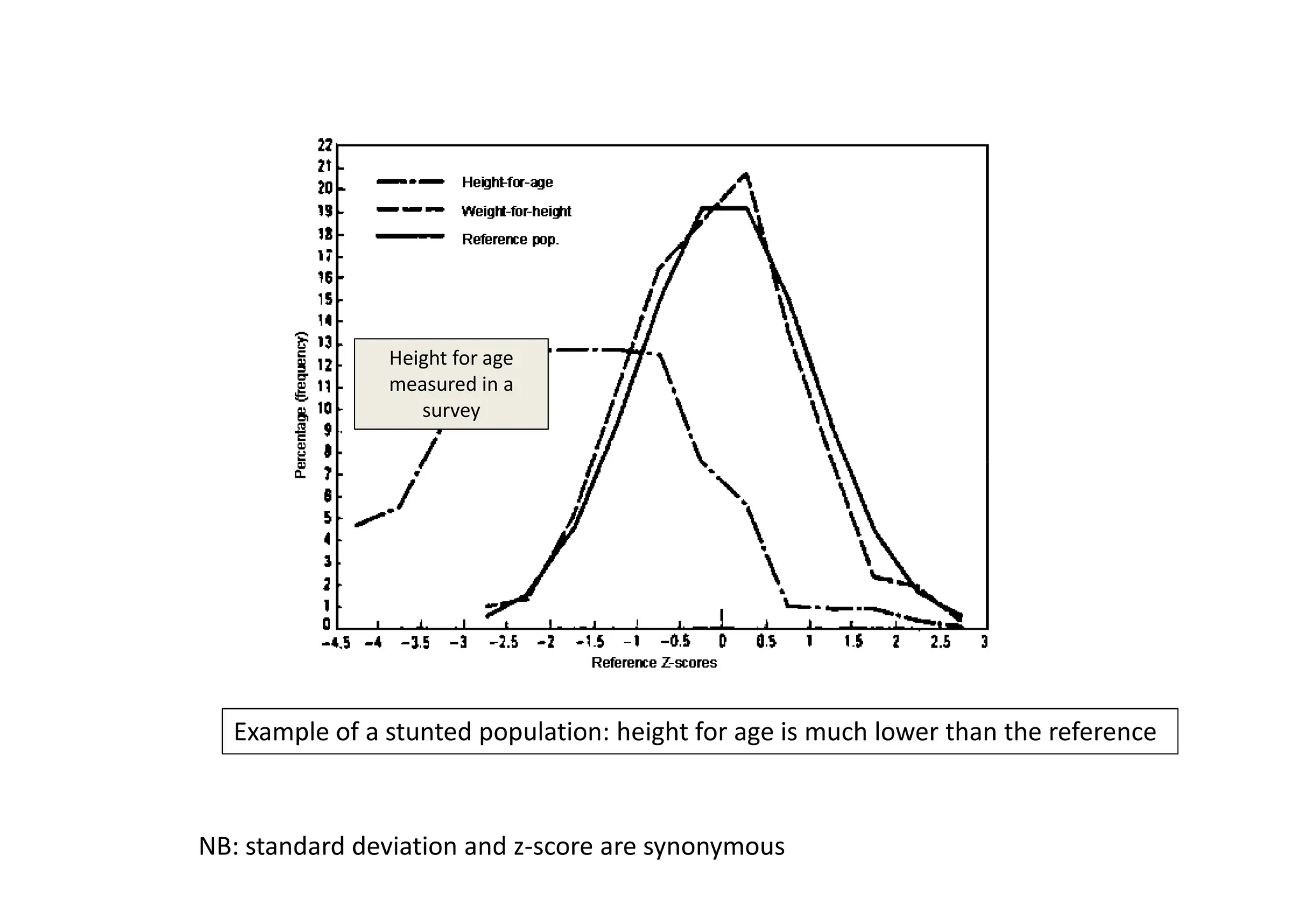
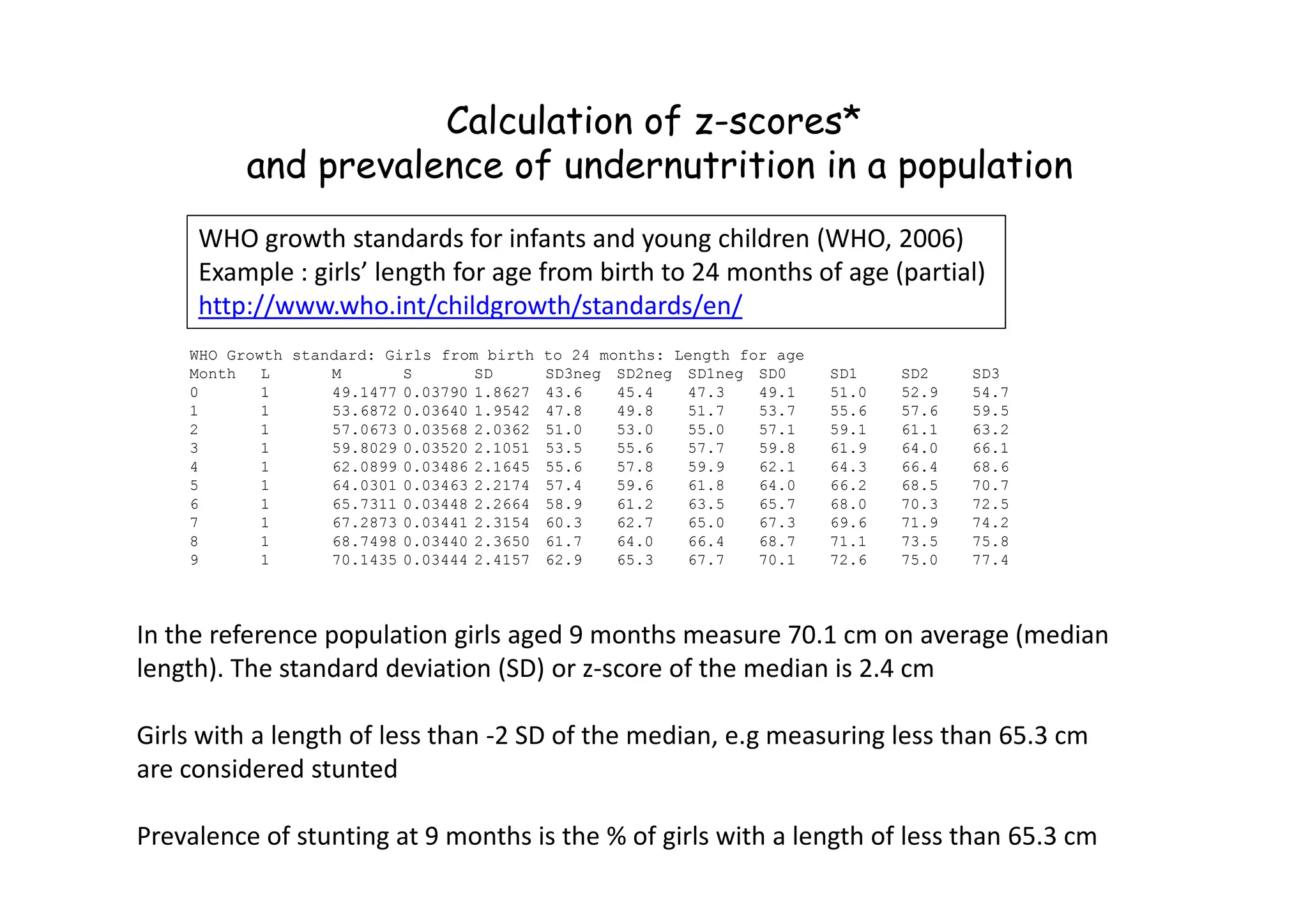
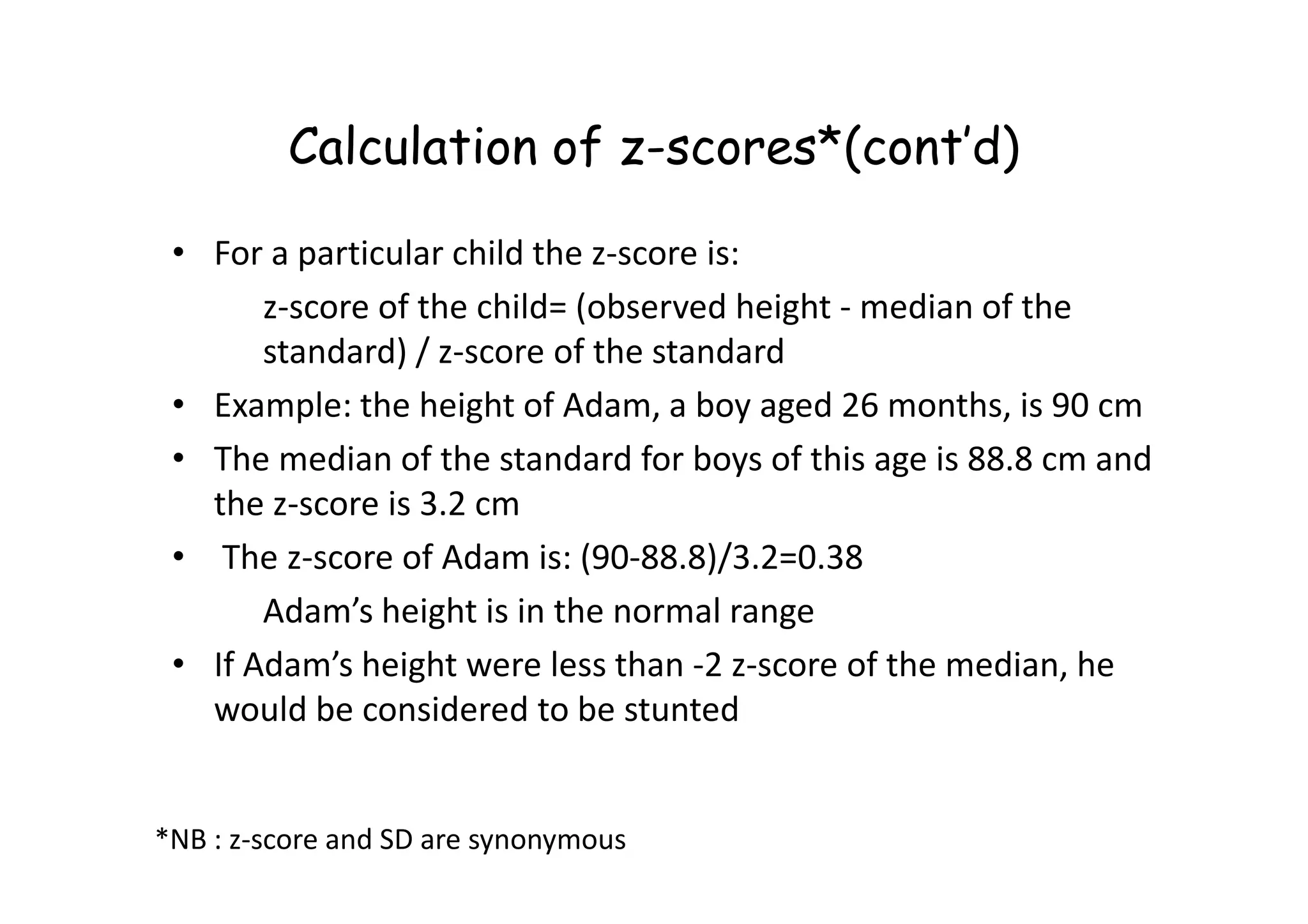
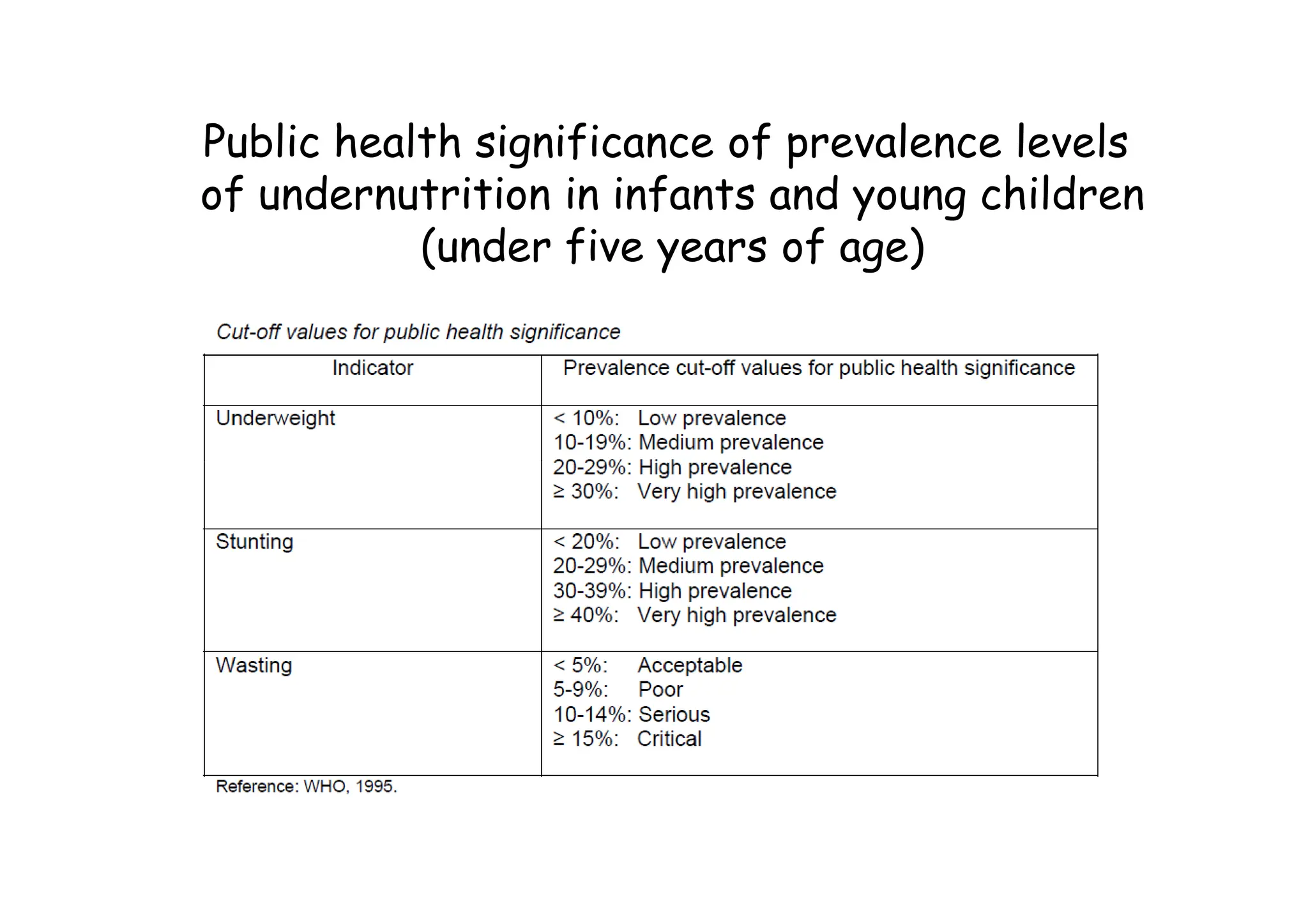
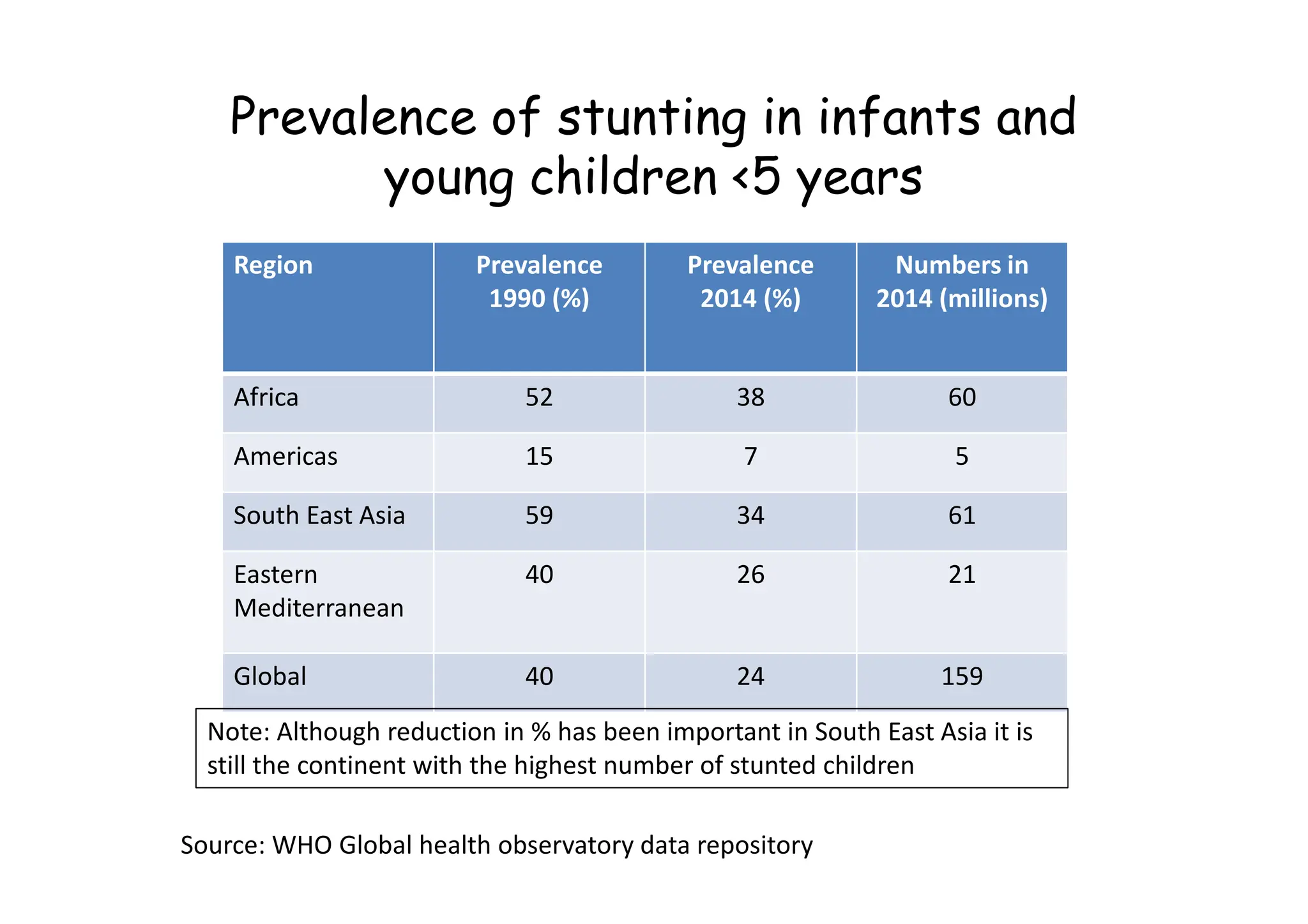
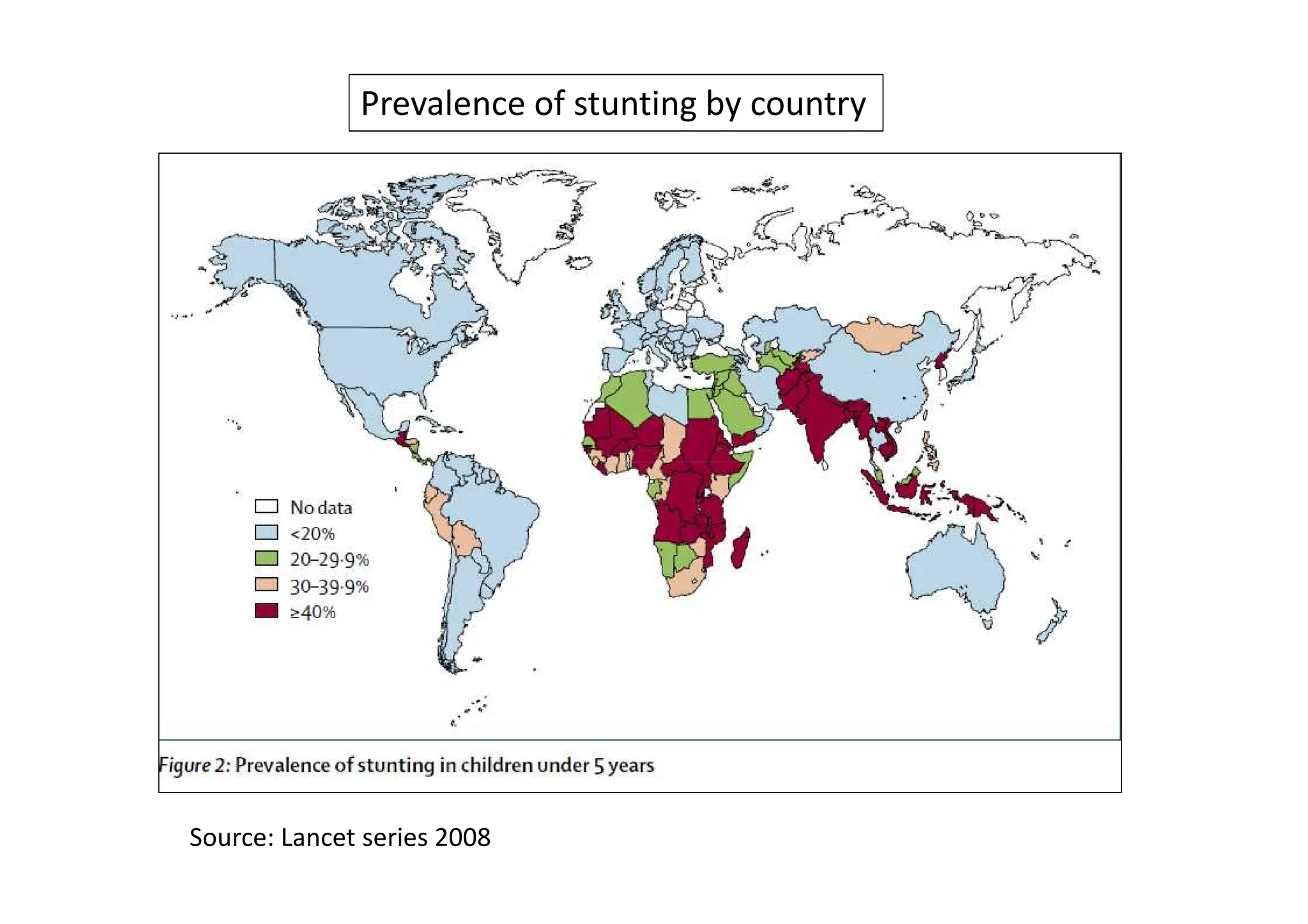
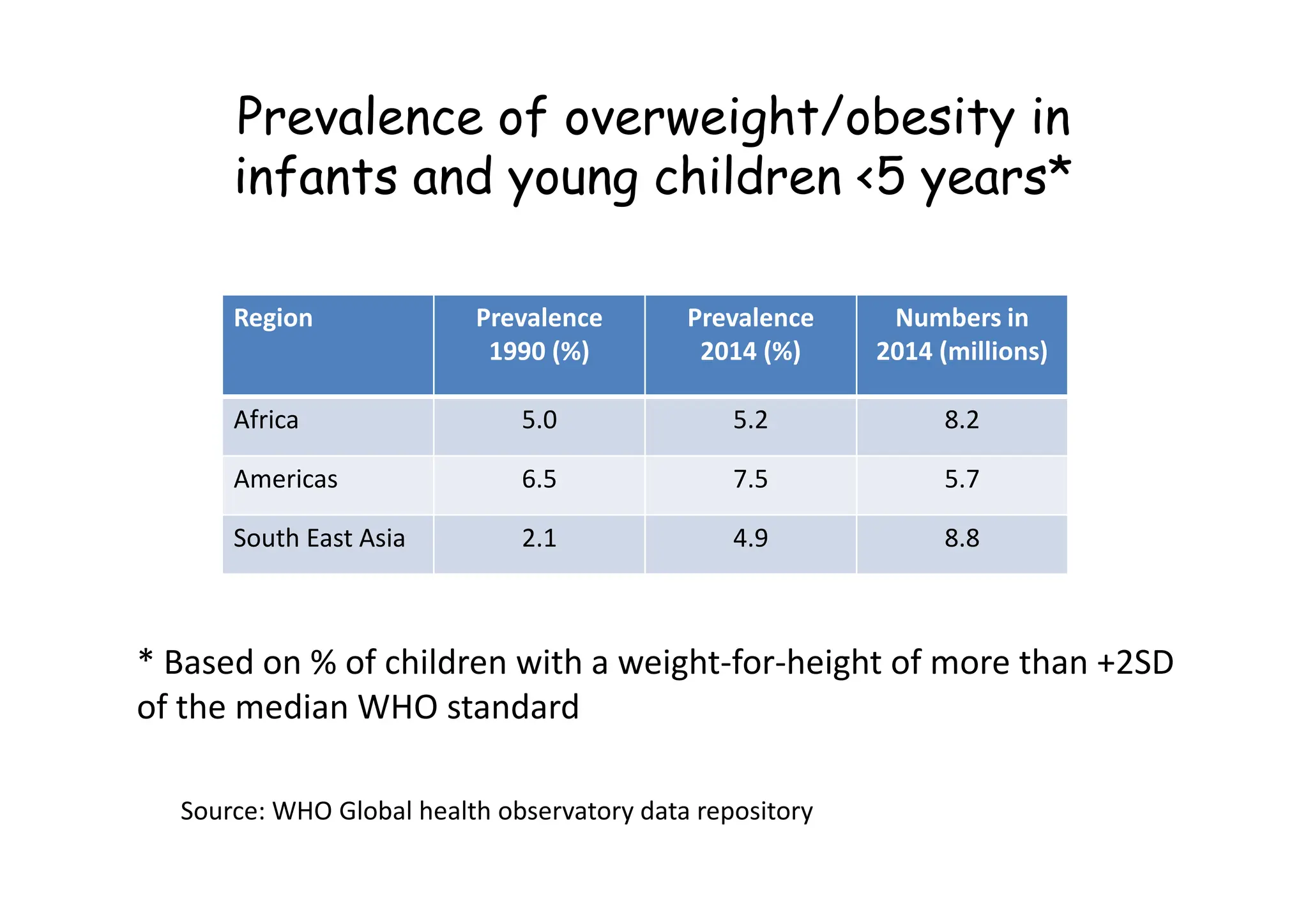
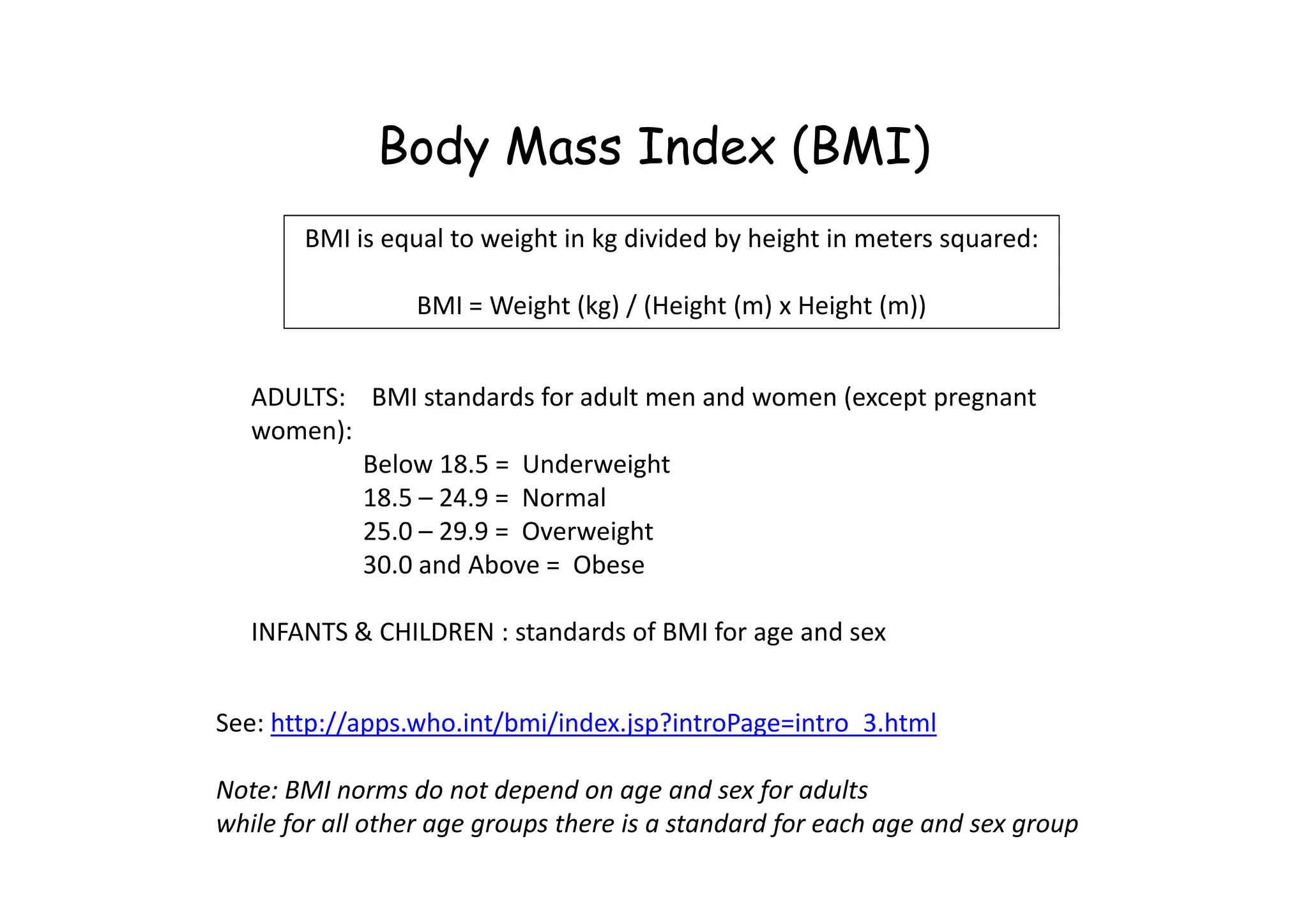
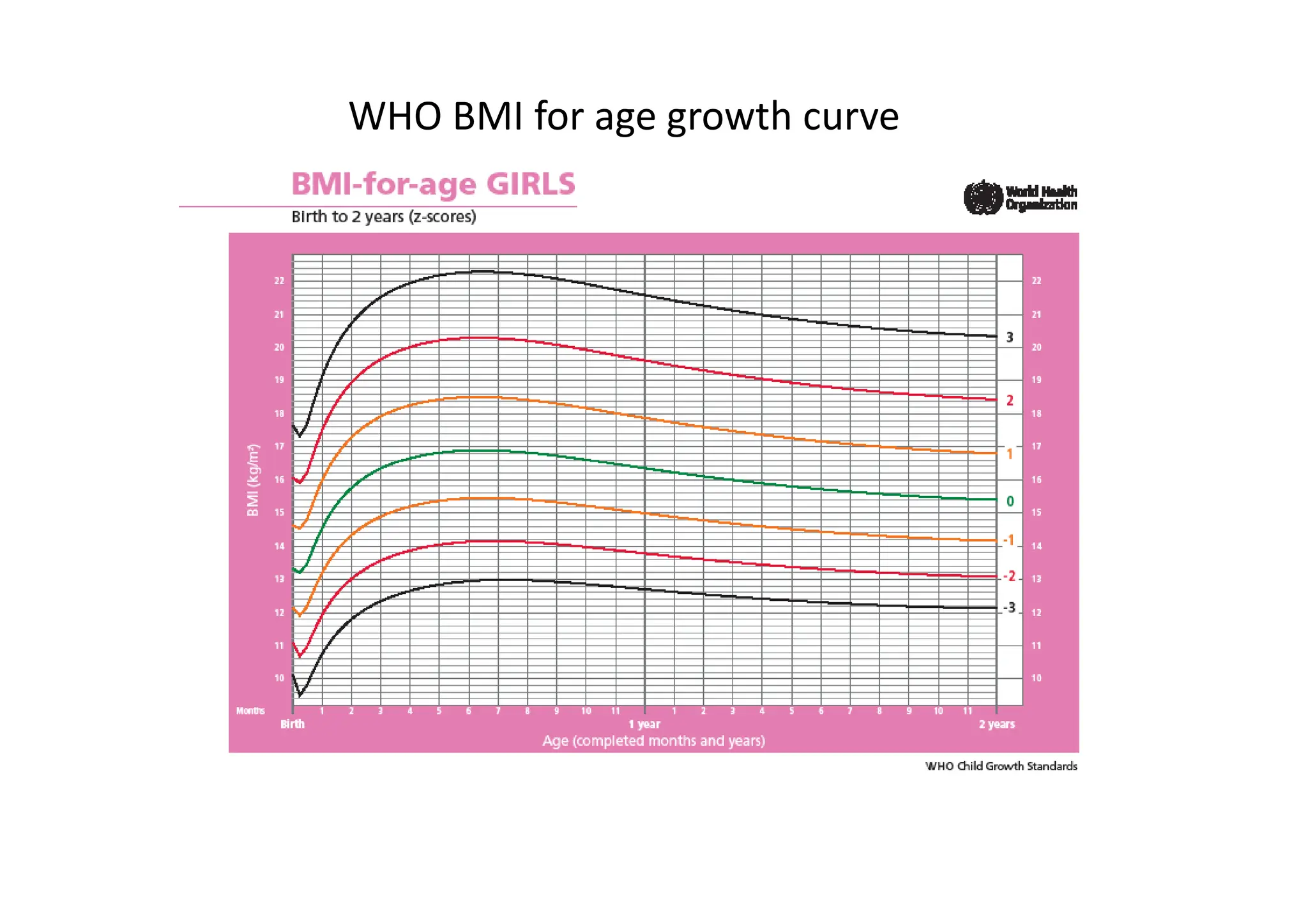
The document discusses malnutrition from a public nutrition perspective, outlining its definition, causes, and assessment indicators. It emphasizes the importance of nutrition in relation to food security and human development, the prevalence of malnutrition globally, and the need for effective monitoring and preventive strategies. Key parts include different types of malnutrition, assessment methods, and the connection between undernutrition and child mortality.