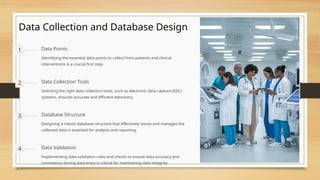
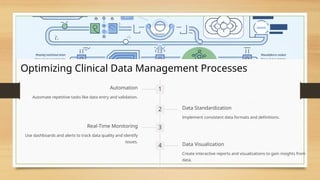
This document provides an overview of clinical data management (CDM), highlighting its importance in ensuring data accuracy, quality, and regulatory compliance in clinical trials. Key responsibilities include data collection, validation, adherence to protocols, and reporting, as well as utilizing technologies like electronic data capture and artificial intelligence to optimize processes. By maintaining data integrity and leveraging emerging technologies, CDM enhances research outcomes and patient safety.