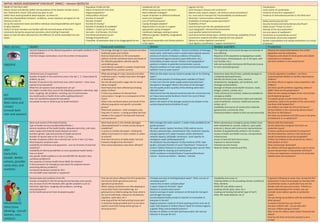
Initial needs assessment checklist for areas affected by a disaster. The checklist includes sections to gather information on: population profiles; livelihoods; logistics; coordination; safety and security; and key sectors including health, food/nutrition, WASH, shelter, and protection. Team members are instructed to choose areas to visit, collect baseline data, verify security conditions, define roles, and agree on how collected data will be assembled into a report. The checklist provides questions to ask key informants and during facility visits in each sector to assess needs, damage, functioning of services and infrastructure, health issues, market conditions, shelter conditions, and protection risks.