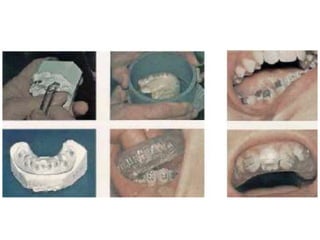
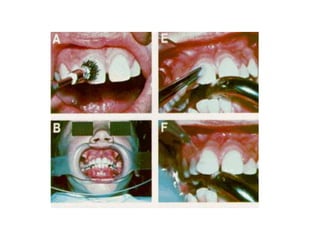
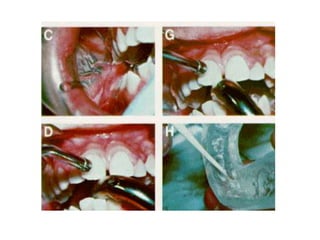
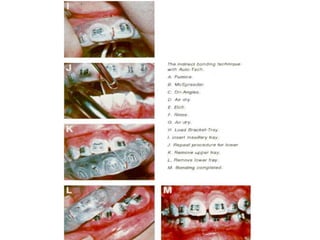
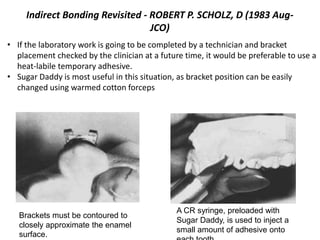
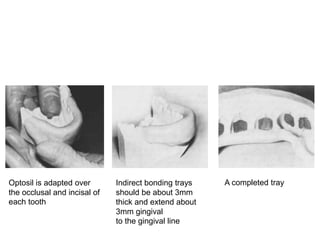
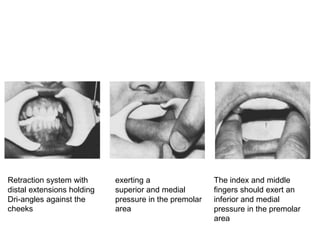
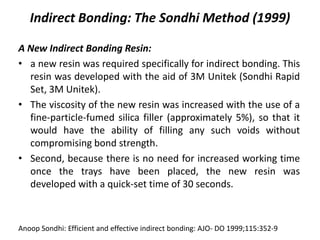
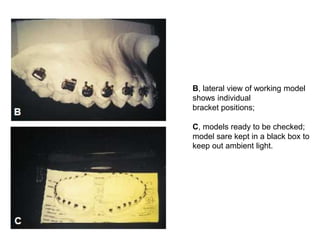
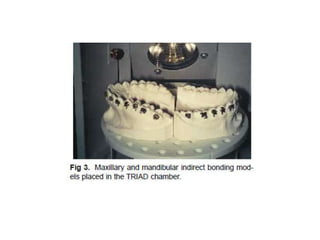
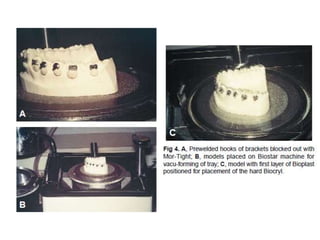
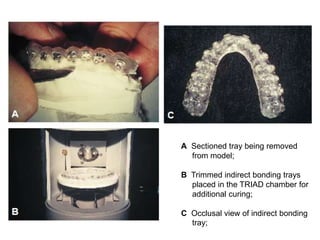
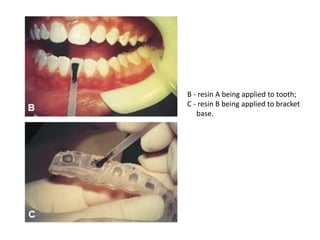
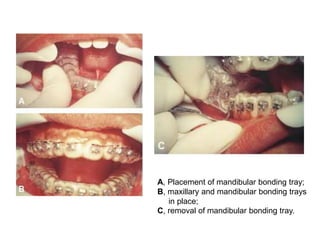
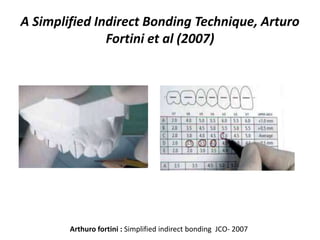
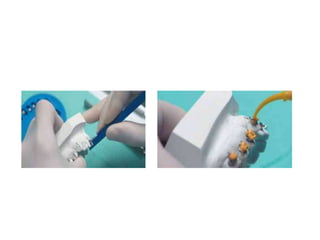
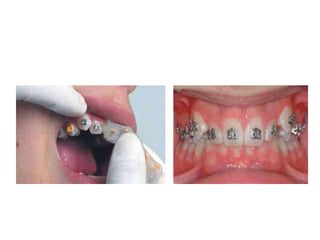
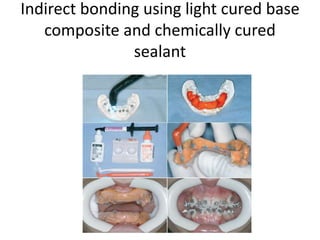
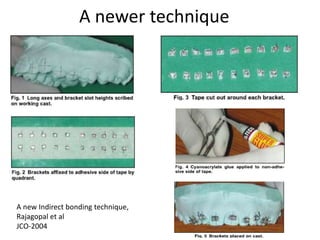
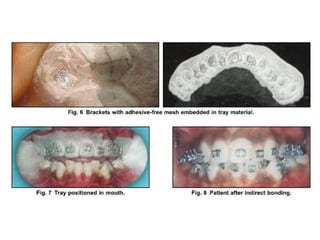
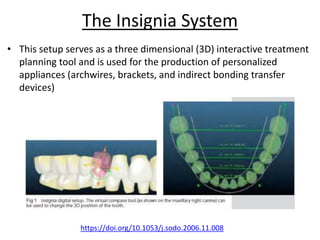
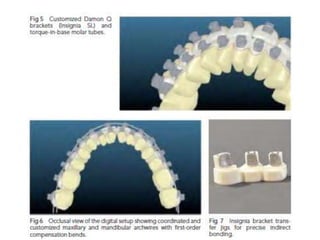
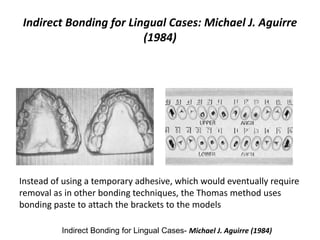
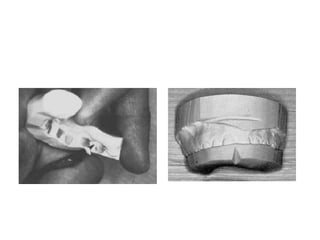
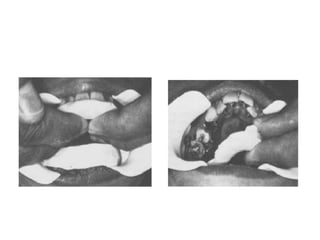
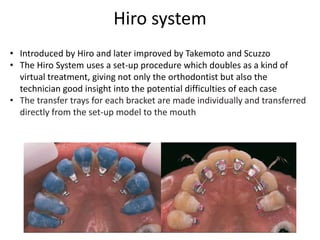
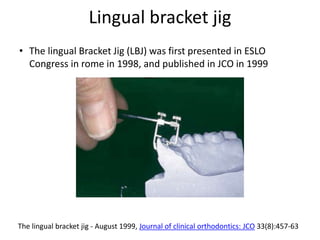
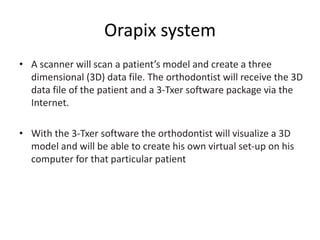
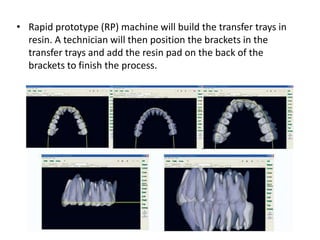
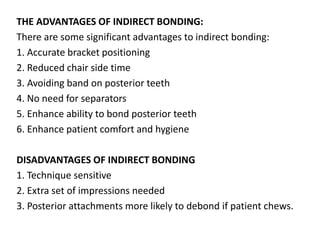
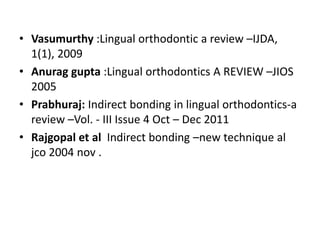
The document discusses indirect bonding techniques in orthodontics, detailing their historical development, advantages, disadvantages, and procedures for both labial and lingual cases. It highlights significant advancements in materials and methods from 1972 to recent years, along with a comparison of bond strengths between direct and indirect bonding. Ultimately, it emphasizes the efficiency and improved outcomes achievable through indirect bonding techniques.