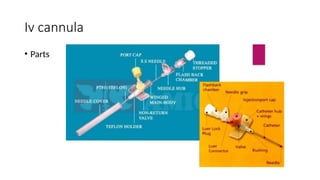
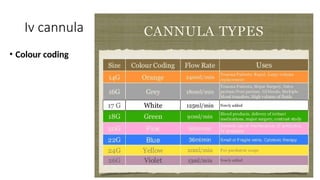
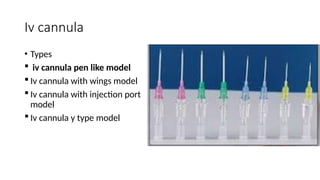
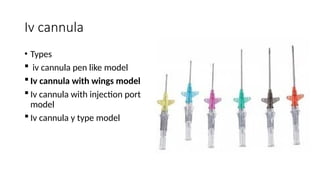
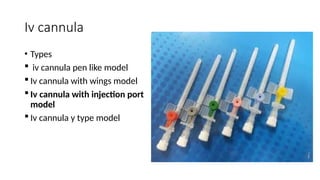
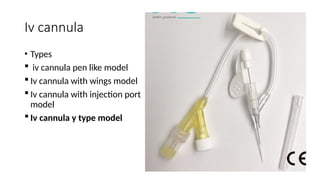
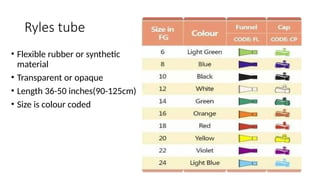
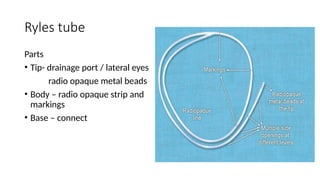
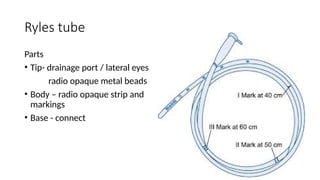
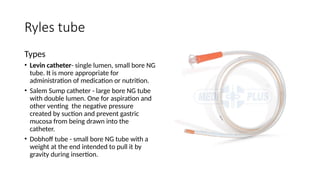
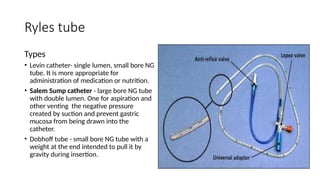
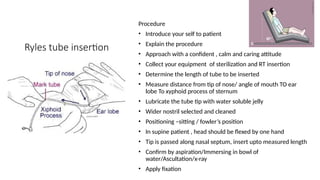
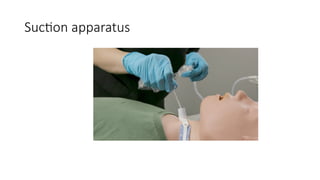
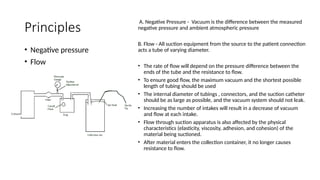
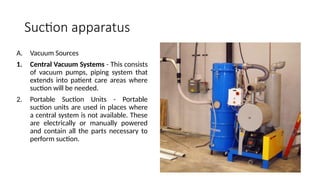
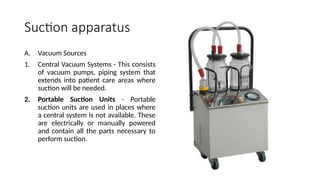
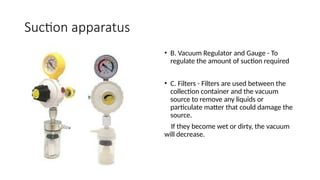
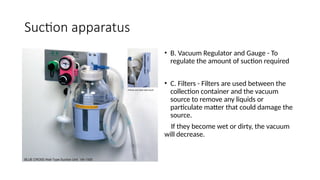
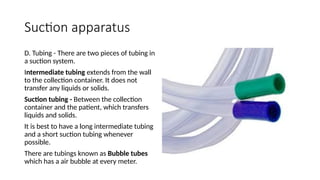
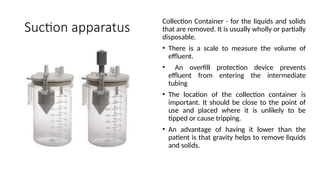
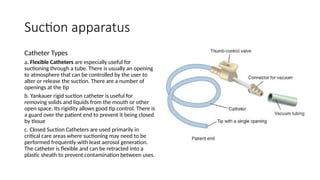
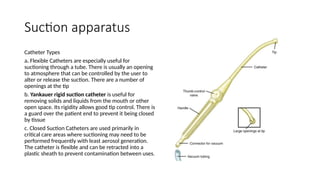
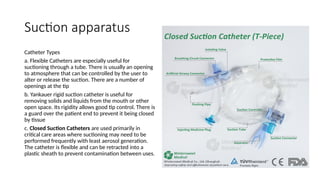
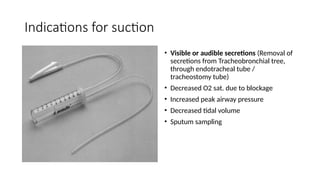
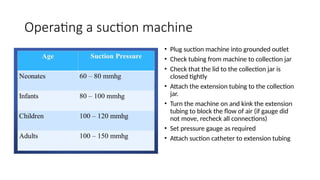
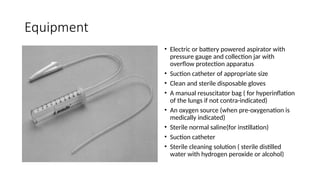
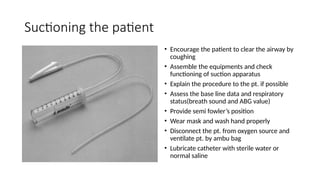
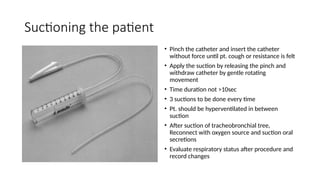
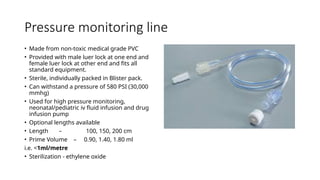
The document provides a detailed overview of various medical procedures and equipment including IV cannulas, Ryles tubes, suction apparatus, and pressure monitoring lines. It outlines insertion procedures, indications, contraindications, complications, and care for each item, emphasizing the importance of proper technique and patient safety. The document also covers sterilization methods and equipment handling protocols essential for healthcare professionals.