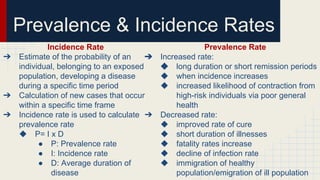
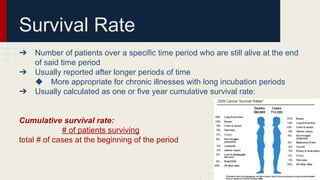
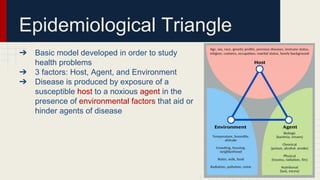
This document defines key concepts in social epidemiology. It discusses how social epidemiology studies the social determinants of health and uses epidemiological methods and social science to promote public health. It defines terms like chronic illness, infectious disease, risk factors, rates of disease prevalence and incidence, and approaches to addressing health disparities. The epidemiological triangle is also introduced as a model for studying disease with factors of the host, agent, and environment.