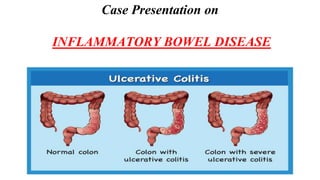
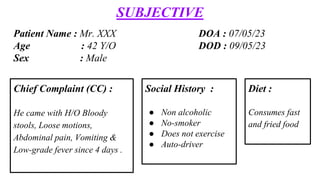
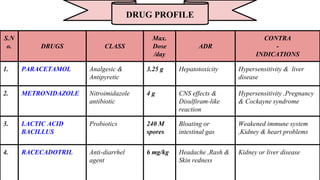
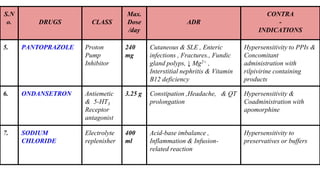
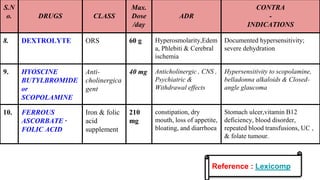
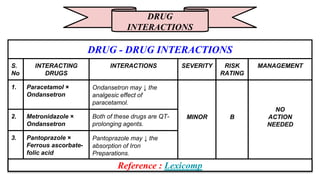
The patient, a 42-year-old male, presented with bloody stools, loose motions, abdominal pain, vomiting and low-grade fever for 4 days. Investigations revealed ulcerative colitis and amoebiasis. He was treated with antipyretics, analgesics, antibiotics, probiotics, anti-diarrheals and electrolyte supplements. His symptoms improved and he was discharged on medications including metronidazole, pantoprazole and ferrous supplements.
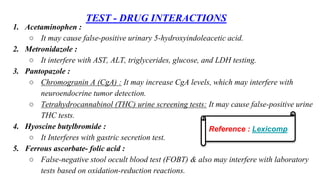
![ASSESSMENT
INTERPRETATION
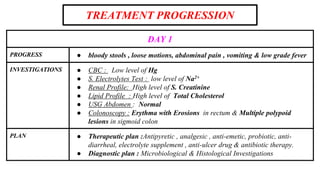
SUBJECTIVE REASON :
● H/O bloody stools, loose motions, abdominal pain, vomiting & low-grade fever since 4
days (CC)
● Consumes fast food and fried diet ( Diet )
● Auto-driver (S/H)
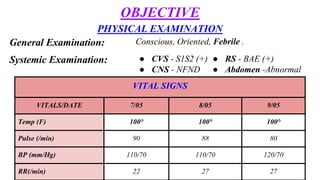
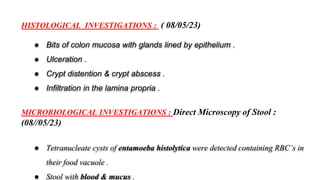
OBJECTIVE EVIDENCE :
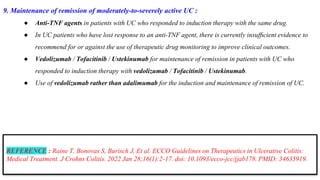
● Fever [100°F] & Abdomen - abnormal (P/E)
● Low levels : Hg (CBC) & Na+ ( electrolytes lab test )
● High levels : S.Cr & T.Cholesterol ( biochemical test )
● +ve of entamoeba histolytica & Stool with blood & mucus ( Microscopy test )
● Ulceration of colon ( Histological test )
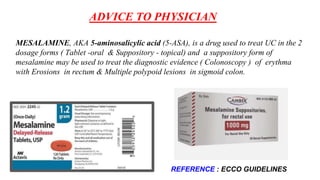
● Erythma with Erosions in rectum & Multiple polypoid lesions in the sigmoid colon (
Colonoscopy )](https://image.slidesharecdn.com/ibdmrs-231114065245-92c39193/85/IBD-Ulcerative-Colitis-9-320.jpg)
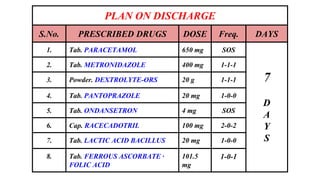
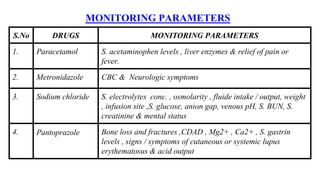
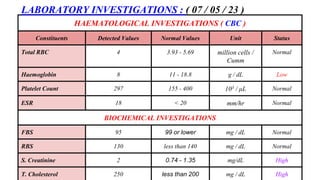
![ECCO Guidelines on Therapeutics in Ulcerative Colitis ( UC )
MEDICAL TREATMENT
1. Induction of remission in patients with mildly-to-moderately active UC :
○ 5-aminosalicylate at a dose of ≥2 g/day
○ Use of colonic-release corticosteroids
1. Induction of remission in patients with active distal colitis :
○ Topical [rectal] 5-ASA at a dose of ≥1g/d.
○ Using topical (rectal steroids.
○ Tx with topical (rectal) 5-ASAS over topical rectal) steroids
○ Use of thiopurines as mono- therapy - Immunomodulators
1. Induction of remission in adult patients with active UC of at least rectosigmoid extent :
○ Use of oral 5-ASA [22 g/d] combined with topical [rectal] 5-ASA over oral 5-ASA
monotherapy](https://image.slidesharecdn.com/ibdmrs-231114065245-92c39193/85/IBD-Ulcerative-Colitis-24-320.jpg)
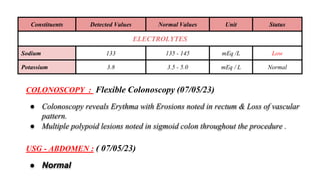
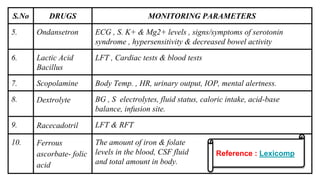
![4. Maintenance of remission in UC patients :
● use of oral 5-ASA at a dose 22 g/day
5. Maintenance of remission in patients with distal UC :
● use of topical rectal 5-ASA
6. Maintenance of remission in patients with steroid- dependent UC or who are intolerant to 5-ASA :
● monotherapy with thiopurines - Immunomodulators
7. Induction of re-mission in non-hospitalised patients with moderately-to-severely active UC :
● Oral prednisolone - systemic corticosteroids
8. Induce remission in patients with moderate-to-severe UC who have inadequate response or intolerance
to conventional therapy :
● Tx with Anti TNF agents [infliximab, adalimumab, and golimumab]
● Vedolizumab - Integrin Receptor Antagonists
● Tofacitinib - Janus Kinase (JAK) Inhibitors
● Ustekinumab - Monoclonal Antibody](https://image.slidesharecdn.com/ibdmrs-231114065245-92c39193/85/IBD-Ulcerative-Colitis-25-320.jpg)