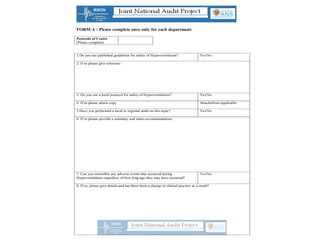
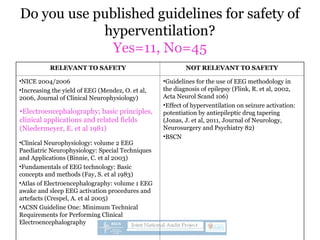
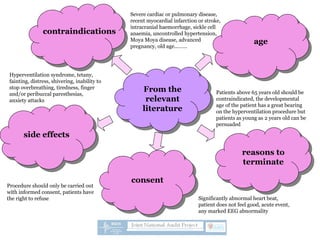
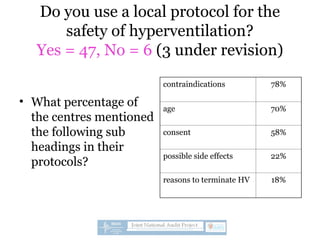
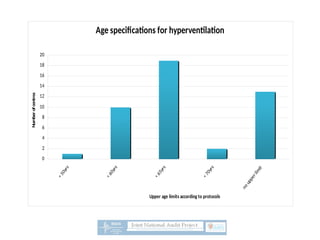
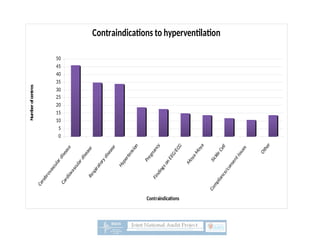
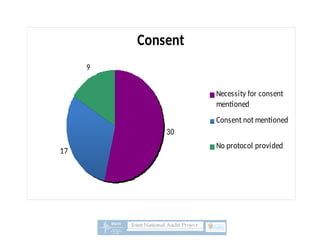
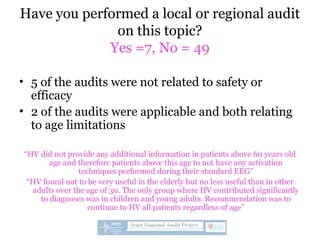
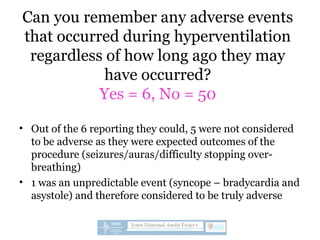
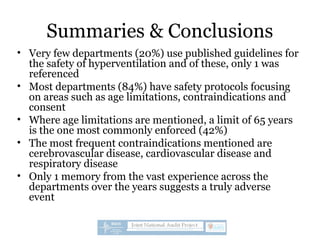
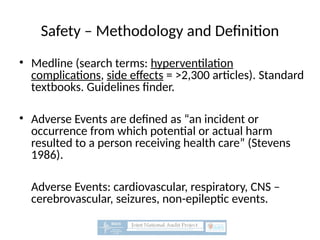
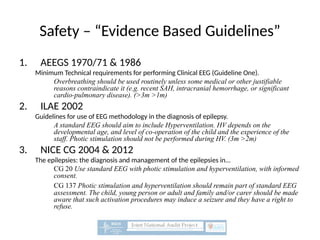
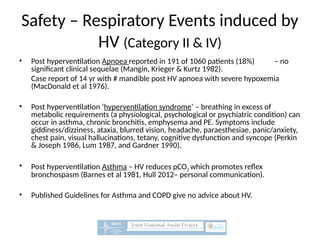
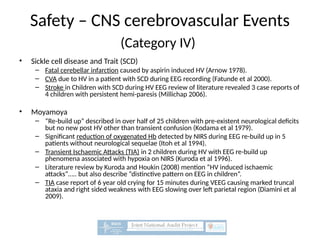
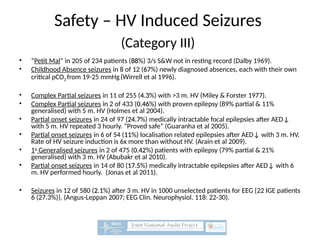
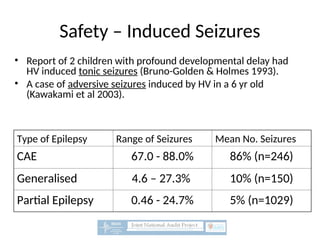
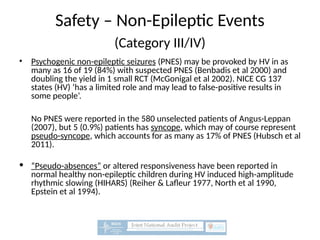
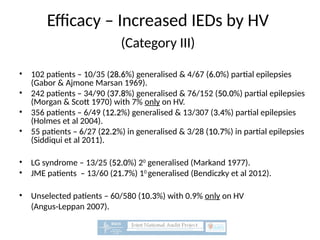
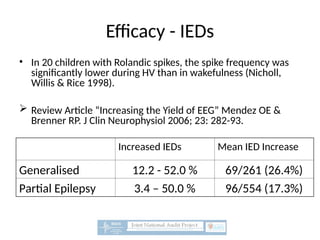
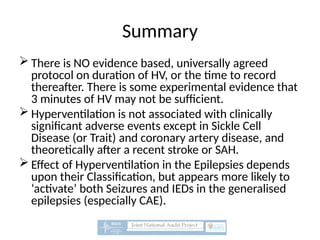
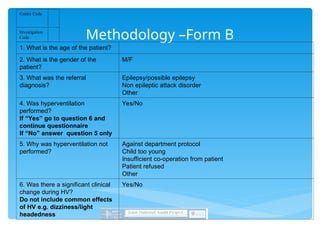
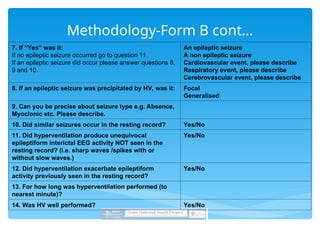
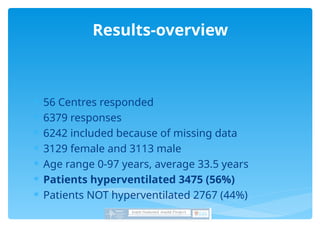
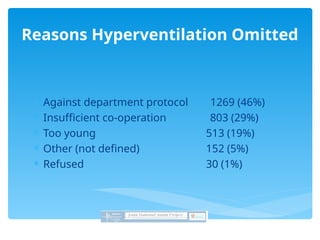
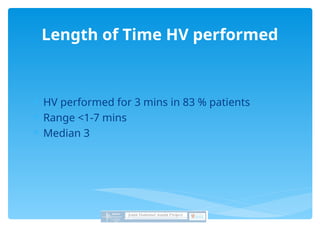
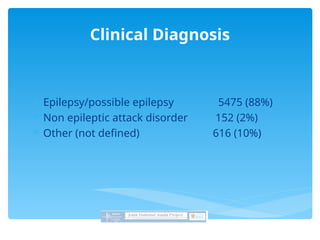
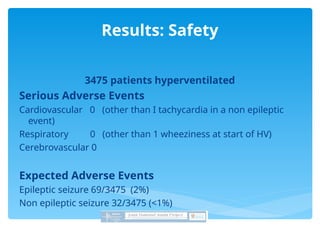
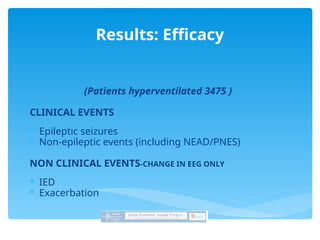
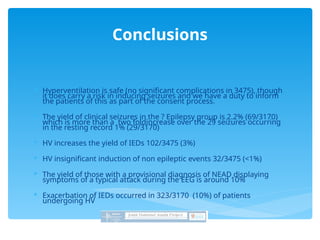
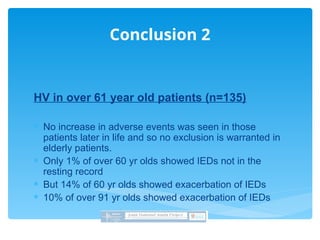
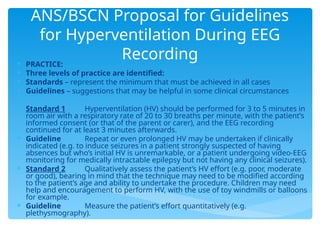
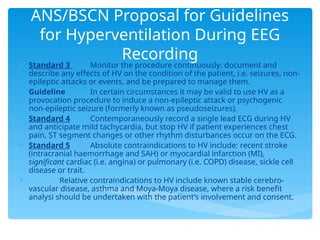
A national survey evaluated the safety and efficacy of hyperventilation during EEG procedures, with a response rate of 89% from 63 forms. Results showed that only 20% of departments utilized published safety guidelines, while 84% had safety protocols addressing age limitations, contraindications, and consent. The survey suggested hyperventilation is generally safe but highlighted the need for more standardized protocols and evidence-based guidelines.