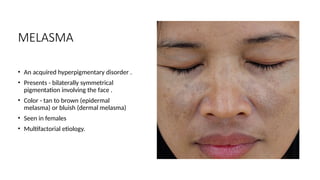
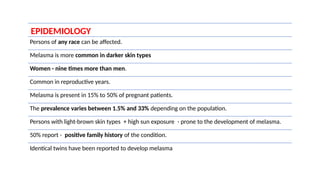
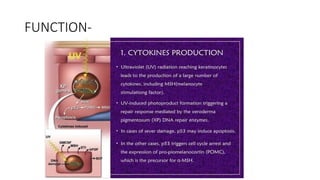
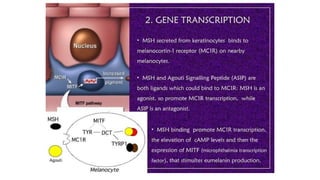
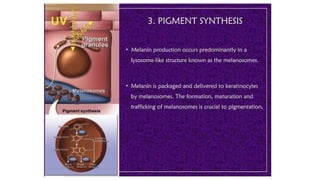
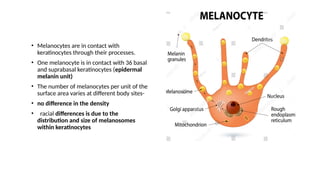
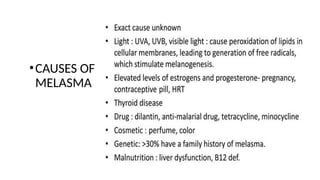
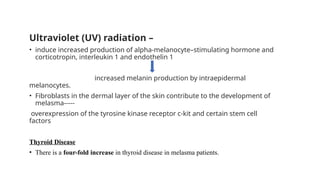
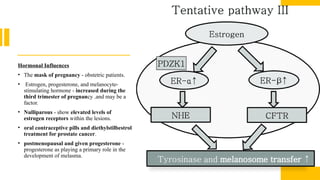
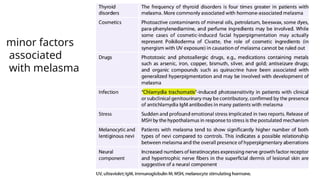
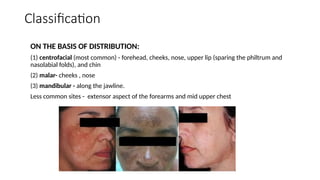
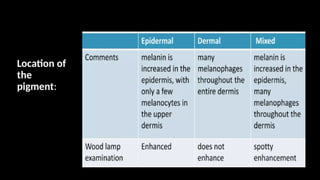
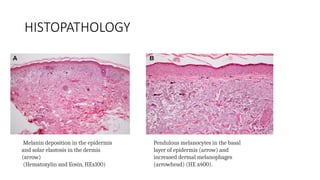
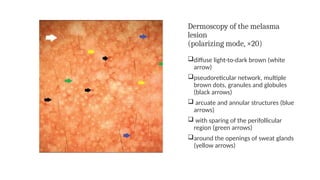
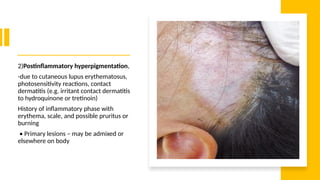
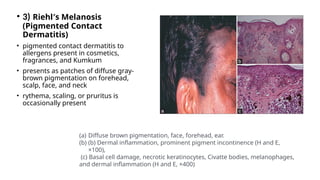
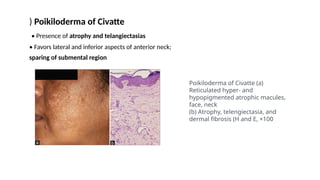
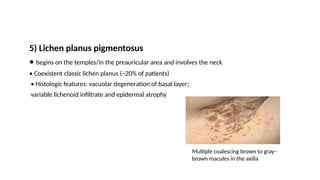
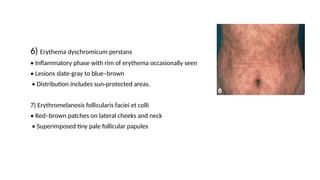
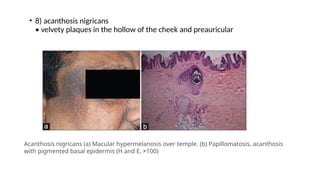
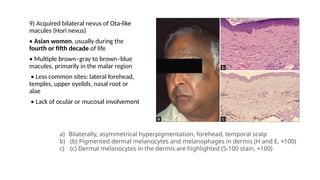
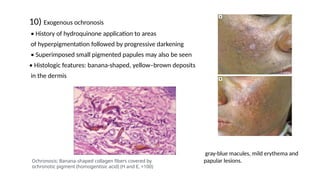
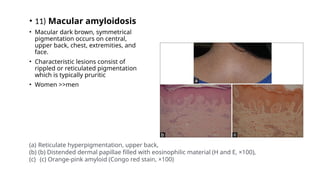
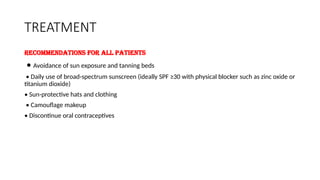
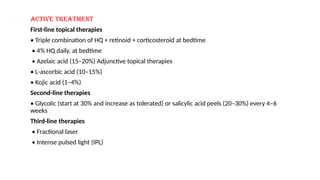
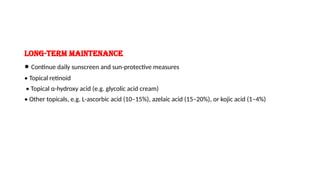
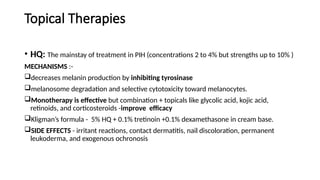
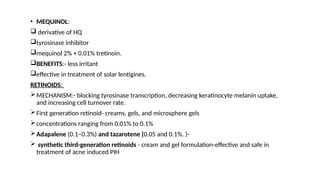
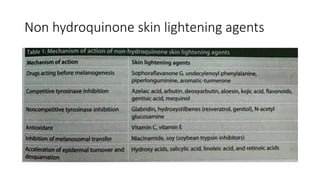
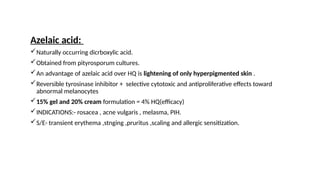
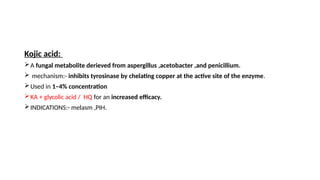
The document provides a comprehensive overview of melasma, an acquired hyperpigmentary disorder characterized by symmetrical facial pigmentation, with a high prevalence in women, particularly during reproductive years and pregnancy. It discusses the multifactorial etiology, including hormonal influences, UV radiation, and genetic predispositions, as well as diagnostic methods and differential diagnoses. Treatment recommendations include sun protection, topical therapies like hydroquinone, and various adjunctive treatments, with an emphasis on customized approaches depending on patient history and melasma characteristics.