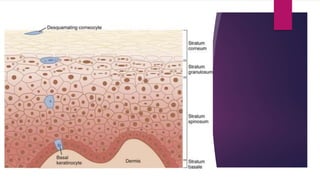
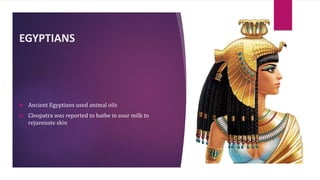
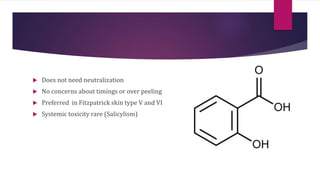
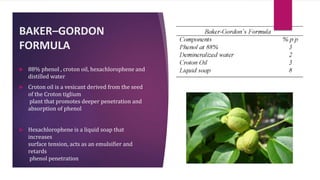
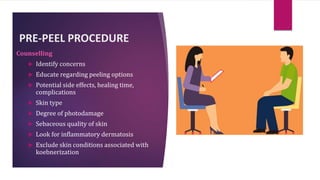
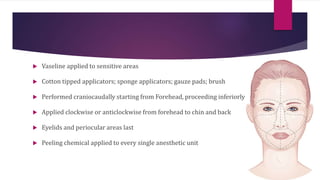
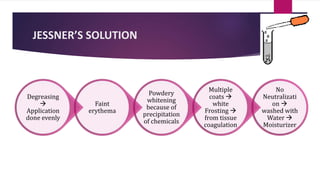
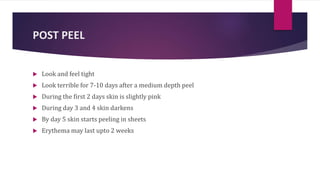
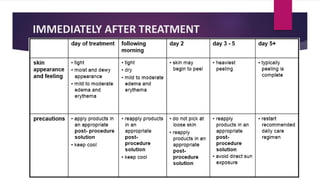
The document provides an overview of chemical peels, including historical uses, types, and their physiological effects on the skin. It details various peeling agents, classifications based on depth, and indications for different skin conditions. Additionally, it outlines procedural steps, post-peel care, potential complications, and specific considerations for patients with skin of color.